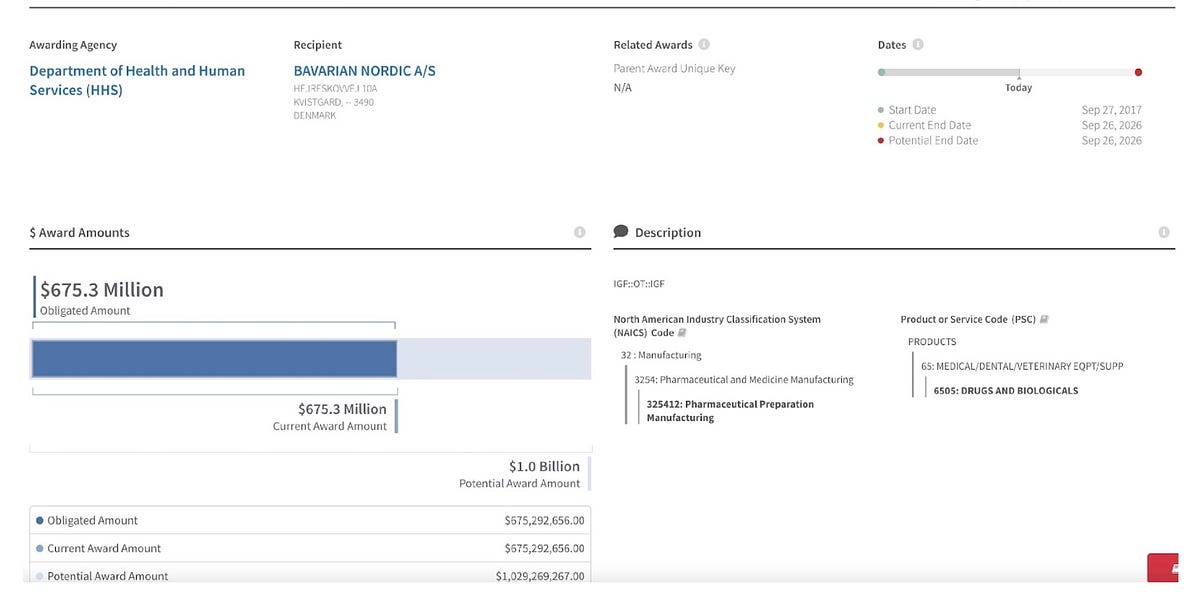
First, I’d like to show you the current $1 billion plus contract for Jynneos, inked in 2017. This came after the contract for the first 20 million doses had been completed, which cost (approximately) a first $Billion. But the USG can’t find the doses.

merylnass.substack.com
(fair use applies)
Monkeypox virus: some truth about the virus and the horribly false solution
The real truth. Some links omitted as they are included in earlier articles by me.
Meryl Nass
16 hr ago
Monkeypox is a real virus that spreads due to skin contact, almost exclusively. If you don’t want to call it a virus, that is okay with me. It is a contagious something that spreads person to person or rarely between animals and humans. If you are not in really closely contact with someone while they are harboring a replicating virus, you won’t get it. Okay, sheets and towels and [smallpox] blankets might spread it, based on experience with smallpox.
The CDC wants to reinvent itself so we can all trust it again. This would require it to produce guidance that is helpful, not harmful, and to be truthful—which it has been unable to do so far, and I don’t think it knows how.
But I can remind the CDC how to make itself useful. Remember the AIDS epidemic, Tony and Rochelle? Aren’t you both supposed to be among America’s top experts on AIDS? That’s your specialty, right?
When NYC faced an HIV epidemic, it closed the bathhouses. It didn’t raise the status of its equity office, Rochelle. Simple, but it made a difference.
Monkeypox is a mild disease but the “pocks” are a great annoyance, because we hate seeing and dealing with them. In some areas, like the mouth and private parts, their downstream effects can be rather painful. The pocks may result in scarring.
Let’s face it: we don’t like dealing with pocks, especially the majority of us who always want to look good. And so the media have taken our distaste and projected it back to us, making the illness appear a lot worse than it actually is. Most cases have only had a few pocks.
The disease (open pocks) lasts from 1-4 weeks. The viral syndrome (fever, malaise) only lasts a few days. CDC said to its ACIP Advisory Committee on June 24 that only symptomatic care is generally needed, and I think that is correct: drink fluids, rest. I don’t think they necessarily want the rest of the population to know that.
I think my case of measles around age 7 was probably worse—I had the things in my mouth and all over my body and eating and drinking was painful and I felt miserable. Here is what my measles looked like:
[picture of a child with the measles]
I am not sure how long people remain contagious with monkeypox; our public health officials have not informed us yet.
From UptoDate:
… until the 2022 outbreak, transmission outside of a household and sustained human-to-human spread had been rare….Viral shedding and period of infectiousness — A person is considered infectious from the onset of clinical manifestations until all skin lesions have scabbed over and re-epithelialization has occurred.
A report of seven cases in the United Kingdom between 2018 and 2021 demonstrated polymerase chain reaction (PCR) positivity in blood and upper respiratory tract samples for at least three weeks in three of the patients. However, it is not clear what this means with respect to infectivity, and the correlation of PCR and culture positivity was not described in the report. Thus, PCR testing of throat or blood samples is generally not done for clinical decision making, and the duration of isolation is determined by clinical evaluation.
Which means, treat the lesions like we treat shingles, cause we don’t really know the duration of contagiousness. If they told us you stop being infectious after a few days or a week, it would seem milder, and the powers that be don’t seem to want that.
Instead the PTB and media are really milking it. For example, writing in depth articles about this serious threat to the nation. Like this one from the WaPo, which is desperately helping the USG to stay on top of the narrative, after I and perhaps others spilled the beans about how much vaccine the USG actually owns. (16 million doses, they say, but it could be more, despending how much has been trashed.) My guess is none has been destroyed and we probably have 30-40 million full doses, some of which may have expired. Sitting frozen in Denmark, hidden from view. Excerpts from the in depth article of August 17 are below, with commentary:
Chaplin [CEO of the Jynneos manufacturer] threatened to cancel all future vaccine orders from the United States, throwing into doubt the administration’s entire monkeypox strategy.
“People are begging for monkeypox vaccines, and we’ve just pissed off the one manufacturer,” said one official who spoke on the condition of anonymity because they were not authorized to comment.
Juice up the story by creating a fake conflict. Make sure it hints of future shortages. CYA by making it anonymous. BTW, this WaPo article includes 3 videos of three gay men showing off their lesions. Because the Yuck! factor is critical to sell the vaccines.
a plodding bureaucracy left hundreds of thousands of gay men facing the threat of an agonizing illness
Nobody has died after 10,000 US cases identified, so it better at least be agonizing. Occasionally.
Demetre Daskalakis, a senior official at the Centers for Disease Control and Prevention, was working from home on HIV prevention projects over the May 14 weekend when CDC colleagues summoned him to an urgent call as cases of unusual lesions had begun to appear in Britain.
Daskalakis quickly brushed up on the symptoms and origins of monkeypox.
“I did the yeoman’s work of getting my infectious-disease biology textbook out and just reviewing stuff about monkeypox to be ready,” Daskalakis said.
Are you impressed? Senior CDC official reads a few paragraphs in a textbook to bone up on monkeypox. What about reading the original literature, bonehead, so you actually might know something, given your responsibility for the entire country’s response?
I have to tell you, I was at a discussion of anthrax about 20-25 years ago with scientists from Fort Detrick and CDC scientists (CDC made the decisions about handling the anthrax letters response). David Ashford and Art Friedlander were there. The CDC people were ignorant about anthrax then; they never had bothered to read the primary literature. That’s why CDC let people keep working in the AMI building in Florida for several days after anthrax was discovered, and minimized the risk to postal workers.
Some things never change.
At the time, the national emergency stockpile held 2,400 doses of Bavarian Nordic’s Jynneos, the only vaccine approved by the Food and Drug Administration for monkeypox. While the United States had purchased millions more potential doses, they sat in Bavarian Nordic’s factory in Denmark, either as finished doses in freezers or as raw materials, waiting to be turned into vaccines.
The U.S. stockpile also had hundreds of millions of shots of an older vaccine approved for the related smallpox virus, ACAM2000, although health officials were wary of using that vaccine — given the increased risk of side effects and even inadvertent illnesses — and considered it a fallback.
But the Jynneos doses in the stockpile were losing shelf life because its freezers were capable of storing the doses only at negative 20 degrees Celsius, while Bavarian Nordic’s freezers in Denmark kept doses stored at negative 50 degrees Celsius.
Before, the media and CDC said the ACAM-2000 stockpile was “at least 100 million.” After I pointed out we bought 300 million doses back in the early 2000s and plenty more since, the story got updated to hundreds of millions. The ACAM-2000 production company is now under the ownership of the anthrax vaccine manufacturer, Emergent BioSolutions. Which means there will be no quality control on vaccine production. This company had to throw away nearly 400 million COVID vaccine doses due to contamination. The taxpayer’s loss. Congress said so: “Committees’ Report on Emergent BioSolutions Uncovers Extensive Vaccine Manufacturing Failures, Deliberate Efforts to Hide Deficiencies. May 10, 2022”
Okay, so the US had already spent around $1.6 billion on the Jynneos vaccine, intended mainly for smallpox, before monkeypox showed up in May. The company had been producing doses for the USG since 2013 or a bit earlier. But the WaPo, the USG mouthpiece, is hinting to us that the government was too cheap to buy the necessary freezers to store it, and that is the excuse why they have been sitting in Denmark? AYFKM?
No, they weren’t kidding.
Shipping the doses would create additional challenges in keeping the vaccines as cold as possible for their 4,000-mile voyage to the United States.
“Every time we move doses from their freezer to the [stockpile] … we lose two years of shelf life,” said Dawn O’Connell, head of the Administration for Strategic Preparedness and Response, which oversees the national stockpile. “Every time we convert doses from [raw materials] to a vial, we lose seven years of shelf life.”
Wait, what? Nearly the entire stockpile of tens of millions of doses has been produced in the past 9 years, and Assistant Secretary of HHS O’Connell just talked about them losing 9 years of shelf life when they get shipped and bottled. Sounds like they must be starting with more than 9 years of shelf life at minus 50 C. Which suggests virtually none of the stockpile expired, after earlier claims that 20 million doses had expired.
Didn’t the USG know this before spending $1.6 Billion to have them manufactured and stored in bulk in Denmark?
Wasn’t the purpose to buy this huge stockpile of vaccine in case of a smallpox emergency? Don’t you need to get it over here pronto when that happens? Like yesterday? Who is blowing smoke by implying there was no plan to rush this stuff from Denmark into arms in days or at most a few weeks, had smallpox occurred?
Early on, every monkeypox test required physicians to first get permission from a city or state epidemiologist, often an hours-long process that required multiple phone calls or emails — before the sample was sent to a public health laboratory, which could take days to release results.
Just like at the start of COVID, CDC controlled all US monkeypox testing. [I don’t know why they did this, but this is one way to control the number of reported cases. And maybe to let it spread more?] Only CDC had the test, and it wasn’t until around July 1 that CDC shipped tests to public health labs and commercial labs and allowed them to do testing as well.
The restrictions created a chokehold: Only about a dozen tests per day were being performed nationwide in early June, at a time when officials believed hundreds or thousands of daily tests were needed to detect infection clusters and head off an outbreak.
Sound familiar?
And communicating the risks of monkeypox to the public was proving to be a challenge, with officials struggling to warn the gay men who were disproportionately contracting the virus, often through sex with multiple partners, while not stigmatizing them.
This stigmatizing BS is a bad joke. Public health officials have been doing contact tracing for syphilis, for example, forever. No one ever said it would stigmatize the polyamorous, or sex workers. All the data are supposed to be strictly confidential. It’s what you do to save lives and prevent fetal malformations. Warn those at risk, dammit. Don’t stigmatize them. Inform them. Keep it confidential. You already have the syphilis protocols and know how to do this. Stop playing coy. Couldn’t CDC come up with a better excuse for not doing its job?
The job today: explain the nation’s plan to split vaccine doses in fifths and administer them with a new injection method, transforming about 441,000 doses of Jynneos into more than 2 million potential shots. The plan was finalized by the FDA over the pharmaceutical company’s safety concerns and after the company backed away from its CEO’s threat to cancel future orders.
So we are ‘unable’ to quickly get the Denmark 16 plus millions of doses shipped and bottled for use. The vaccine is fully licensed and legally could very well have liability attached to it if injuries occur (and plenty will-I previously wrote about very high numbers of recipients in the clinical trials with elevated cardiac enzymes and worsening HIV status). Hello Rochelle and Tony, was this deliberate? Instead of worrying about stigmatizing, are you warning HIV positive people that the vaccine is known to cause higher HIV virus titers and lower CD4 counts?
And then there is this: the USG is ‘able’ to get the already bottled doses sucked out of vials, diluted and totally rebottled as diluted product, never having undergone testing of the process, whether it works, whether the dose makes sense. The administration announced it will be doing that, which is not simple.
But they can’t just defrost and bottle the bulk vaccine? Seems to me it is a lot more complicated to remove, dilute and rebottle than to simply bottle what we already own. Especially since we own plenty. Buy the freezers, ship the stuff over, and have US companies bottle it. That is, if we really need it and this whole thing is not a clown show.
The diluted product got an EUA on August 9, which removes essentially all liability. How convenient. Maybe that is why the USG is diluting it? Or will they just bottle the old vaccine, call it diluted, and still get the liability waiver?
BTW, the intradermal injection method is the exact same method used when doing a TB test. Not hard to learn or to do.
So many gay men across the country still struggling to get vaccinated. A second dose needed 28 days after the first shot. At least 14 days after the second dose for full protection.
Full protection? STAT, as I previously noted, recently carried an Op-Ed by 2 former top officials at FDA on the monkeypox vaccines. They revealed that the Jynneos vaccine does not prevent transmission! It supposedly reduces severity of the disease.
Where have we heard that before? Go get vaccinated, risk myocarditis or a worsening of HIV, wait 42 days for “full protection” from a diluted dose (or not) that has never been tested in humans—and then find out you can still catch and spread monkeypox.
Fool me once, shame on you. Fool me twice…
UPDATE Aug 20:
Breakthrough monkeypox cases emerge
Breakthrough monkeypox cases emerge
Preliminary reports on monkeypox vaccinations suggest the vaccine is not 100 percent effective, and some breakthrough cases are occurring, the World Health Organization said during an Aug. 17 media briefing.
In some cases, breakthrough infections are occurring in people vaccinated after a monkeypox exposure, which is intended to reduce disease severity. The breakthrough cases should not come as a surprise, as the WHO was not expecting 100 percent efficacy, according to Dr. Rosamund Lewis, the organization's technical lead for monkeypox. [Is it a surprise to the gay men lining up for hours for a shot at the shot?—Nass]
"We have known from the beginning that this vaccine would not be a silver bullet, that it would not meet all the expectations that are being put on it, and that we don't have firm efficacy data or effectiveness data in this context," she said.
Dr. Lewis cited a limited study from the 1980s, which showed that smallpox vaccines used at the time were about 85 percent effective against monkeypox. [It used a different vaccine, believed to be much more effective than Jynneos, however.—Nass]
She said it's unclear what the current vaccine's overall efficacy will be, but still stressed the importance of vaccination to protect those at high risk.