You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
MNKYPOX Monkeypox - Consolidated Thread.
- Thread starter Tigerlily
- Start date
TammyinWI
Talk is cheap
AIDS all over again... on purpose, spread by the 'special class' of individuals. Rainbows and Unicorns for all.
Yeah, and I wonder if them dang "vaccines" cause it to flare up in people, and also can cause the person who takes it to "shed" on others around them, and they will claim that it is not just catchy through sex.
BenIan
Veteran Member
View: http://twitter.com/catparkerphoto/status/1561992153718562816?s=21&t=hg_VfHaOPR1yvAUsAIf0qQ
This lady says it’s a vaccine side effect. Posting here for picture comparison.
This lady says it’s a vaccine side effect. Posting here for picture comparison.
psychgirl
Has No Life - Lives on TB
UmmmView: http://twitter.com/catparkerphoto/status/1561992153718562816?s=21&t=hg_VfHaOPR1yvAUsAIf0qQ
This lady says it’s a vaccine side effect. Posting here for picture comparison.
Is it monkeypox, or that autoimmune blistering that’s been mentioned regarding Covid shot??
inskanoot
Veteran Member
NBC has an article that came out yesterday, which I found through reading the thread on the poor dog that got monkeypox.
Interestingly, NBC will not allow copy/pasting of this article.
But is is a medical study, recently completed by at least three different groups of doctors, indicating that monkey pox is NOT transmitted merely by "skin contact" but by the transmission of semen in sexual intercourse. Links are given in the article.
I paste below the link, title, and introductory teaser--it is all the site will allow me to paste.

Sex between men, not skin contact, is fueling monkeypox, new research suggests
The claim that skin-to-skin contact during sex between men, not intercourse itself, drives most monkeypox transmission is likely backward, a growing group of experts say.www.nbcnews.com
Sex between men, not skin contact, is fueling monkeypox, new research suggests
The claim that skin-to-skin contact during sex between men, not intercourse itself, drives most monkeypox transmission is likely backward, a growing group of experts say.
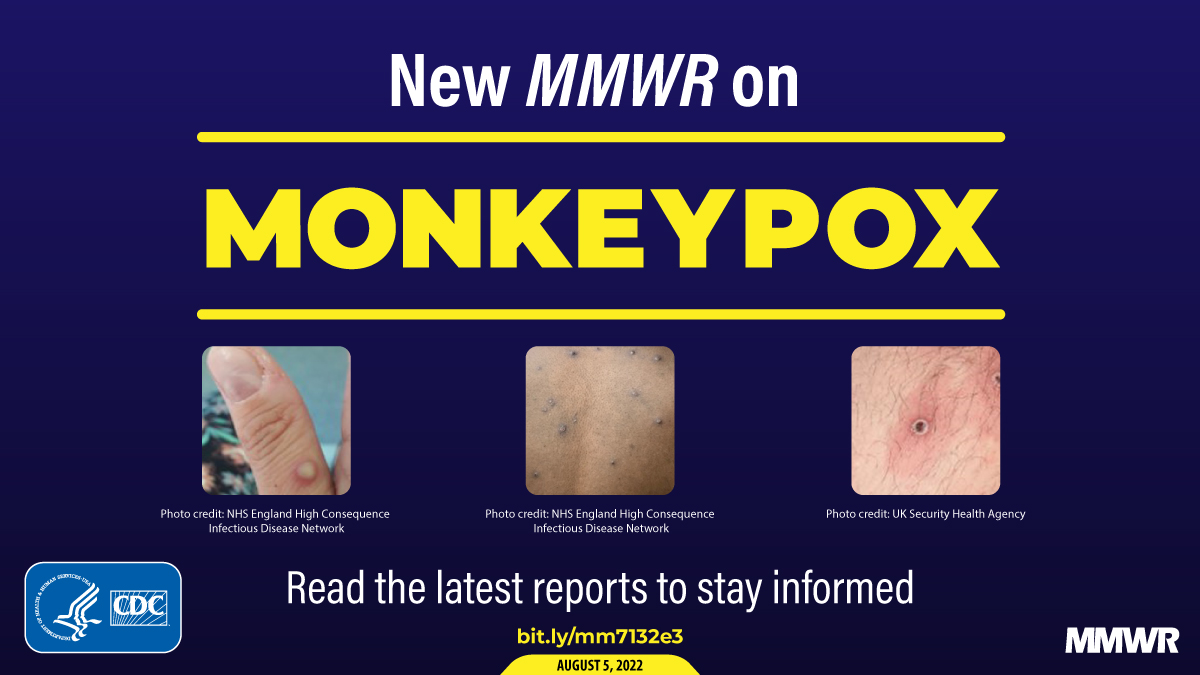
Epidemiologic and Clinical Characteristics of Monkeypox Cases...
This report describes the epidemiologic and clinical characteristics of monkeypox cases reported to CDC by July 22, 2022.
Partial:
Epidemiologic and Clinical Characteristics of Monkeypox Cases — United States, May 17–July 22, 2022
Weekly / August 12, 2022 / 71(32);1018-1022On August 5, 2022, this report was posted online as an MMWR Early Release.
David Philpott, MD1,2; Christine M. Hughes, MPH2; Karen A. Alroy, DVM3; Janna L. Kerins, VMD4; Jessica Pavlick, DrPH5; Lenore Asbel, MD6; Addie Crawley, MPH3; Alexandra P. Newman, DVM7; Hillary Spencer, MD1,4; Amanda Feldpausch, DVM5; Kelly Cogswell, MPH8; Kenneth R. Davis, MPH9; Jinlene Chen, MD10; Tiffany Henderson, MPH11; Katherine Murphy, MPH12; Meghan Barnes, MSPH13; Brandi Hopkins, MPH14; Mary-Margaret A. Fill, MD15; Anil T. Mangla, PhD16; Dana Perella, MPH6; Arti Barnes, MD17; Scott Hughes, PhD3; Jayne Griffith, MPH18; Abby L. Berns, MPH19; Lauren Milroy, MPH20; Haley Blake, MPH21; Maria M. Sievers, MPH22; Melissa Marzan-Rodriguez, DrPH23; Marco Tori, MD1,24; Stephanie R. Black, MD4; Erik Kopping, PhD3,25; Irene Ruberto, PhD26; Angela Maxted, DVM, PhD27; Anuj Sharma, MPH5; Kara Tarter, MPH28; Sydney A. Jones, PhD29,30; Brooklyn White, MPH31; Ryan Chatelain, MPH32; Mia Russo; Sarah Gillani, MPH16; Ethan Bornstein, MD1,8; Stephen L. White, PhD9; Shannon A. Johnson, MPH11; Emma Ortega, MPHTM12; Lori Saathoff-Huber, MPH17; Anam Syed, MPH5; Aprielle Wills, MPH3; Bridget J. Anderson, PhD7; Alexandra M. Oster, MD2; Athalia Christie, DrPH2; Jennifer McQuiston, DVM2; Andrea M. McCollum, PhD2; Agam K. Rao, MD2,*; María E. Negrón, DVM, PhD2,*; CDC Multinational Monkeypox Response Team (View author affiliations)
View suggested citation
Summary
What is already known about this topic?A global monkeypox outbreak began in 2022.
What is added by this report?
Among U.S. monkeypox cases with available data, 99% occurred in men, 94% of whom reported recent male-to-male sexual or close intimate contact; racial and ethnic minority groups appear to be disproportionately affected. Clinical presentations differed from typical monkeypox, with fewer persons experiencing prodrome and more experiencing genital rashes.
What are the implications for public health practice?
Public health efforts should prioritize gay, bisexual, and other men who have sex with men, who are currently disproportionately affected, for prevention and testing, address equity, and minimize stigma, while maintaining vigilance for transmission in other populations. Clinicians should test persons with rash consistent with monkeypox, regardless of whether the rash is disseminated or was preceded by prodrome.
Monkeypox, a zoonotic infection caused by an orthopoxvirus, is endemic in parts of Africa. On August 4, 2022, the U.S. Department of Health and Human Services declared the U.S. monkeypox outbreak, which began on May 17, to be a public health emergency (1,2). After detection of the first U.S. monkeypox case), CDC and health departments implemented enhanced monkeypox case detection and reporting. Among 2,891 cases reported in the United States through July 22 by 43 states, Puerto Rico, and the District of Columbia (DC), CDC received case report forms for 1,195 (41%) cases by July 27. Among these, 99% of cases were among men; among men with available information, 94% reported male-to-male sexual or close intimate contact during the 3 weeks before symptom onset. Among the 88% of cases with available data, 41% were among non-Hispanic White (White) persons, 28% among Hispanic or Latino (Hispanic) persons, and 26% among non-Hispanic Black or African American (Black) persons. Forty-two percent of persons with monkeypox with available data did not report the typical prodrome as their first symptom, and 46% reported one or more genital lesions during their illness; 41% had HIV infection. Data suggest that widespread community transmission of monkeypox has disproportionately affected gay, bisexual, and other men who have sex with men and racial and ethnic minority groups. Compared with historical reports of monkeypox in areas with endemic disease, currently reported outbreak-associated cases are less likely to have a prodrome and more likely to have genital involvement. CDC and other federal, state, and local agencies have implemented response efforts to expand testing, treatment, and vaccination. Public health efforts should prioritize gay, bisexual, and other men who have sex with men, who are currently disproportionately affected, for prevention and testing, while addressing equity, minimizing stigma, and maintaining vigilance for transmission in other populations. Clinicians should test patients with rash consistent with monkeypox,† regardless of whether the rash is disseminated or was preceded by prodrome. Likewise, although most cases to date have occurred among gay, bisexual, and other men who have sex with men, any patient with rash consistent with monkeypox should be considered for testing. CDC is continually evaluating new evidence and tailoring response strategies as information on changing case demographics, clinical characteristics, transmission, and vaccine effectiveness become available.§
On June 3, 2022, CDC released a case report form for health departments to report monkeypox cases. Data collected include possible exposures during the 3 weeks preceding symptom onset, symptoms during the illness course, and distribution of rash, defined as at least one lesion on the skin or mucous membranes. To describe epidemiologic and clinical characteristics, CDC analyzed case report form data for probable or confirmed cases¶ initially reported through July 22, 2022; to allow for reporting delay, data received through July 27 were included. Analyses were restricted to cases for which relevant data were available. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.**
During May 17–July 22, 2022, a total of 2,891 U.S. monkeypox cases were reported by 43 states, Puerto Rico, and DC; the number of reported cases increased rapidly during this time (Figure). Case report forms including, at minimum, age and gender identity were received for 1,195 (41%) cases; these cases are described in this report. Median age was 35 years (IQR = 30–41 years). Nearly all (99%) persons with case report forms available were men (cisgender and transgender) (Table 1). Among 1,054 cases for which race and ethnicity were reported, 41% occurred among White persons, 28% among Hispanic persons, and 26% among Black persons. Based on information available in case report forms, the percentage of cases among Black persons increased from 12% (29 of 248) during May 17–July 2 to 31% (247 of 806) during July 3–22, and the percentage among Hispanic persons decreased from 33% (82 of 248) to 27% (214 of 806) and among White persons from 49% (121 of 248) to 38% (307 of 806).
Among 241 cases (20%) with reported classification by health departments as being travel-associated or locally acquired, 178 (74%) were classified as locally acquired. The percentage of locally acquired cases increased from 51% (33 of 65) during May 17–July 2 to 82% (145 of 175) during July 3–22.
Among 358 (30%) men (cisgender and transgender) with information on recent sexual behaviors and gender of sex partners available, 337 (94%) reported sex or close intimate contact with a man during the 3 weeks before symptom onset; 16 (4%) reported no such contact. Among 291 men who reported information about their male sexual partners during the 3 weeks preceding symptom onset, 80 (27%) reported one partner, 113 (40%) reported two to four partners, 42 (14%) reported five to nine partners, and 56 (19%) reported 10 or more partners. Among 86 men with information reported, 33 (38%) reported group sex, defined as sex with more than two persons, at a festival, group sex event, or sex party.
The most frequently reported signs and symptoms included rash (100%), fever (63%), chills (59%), and lymphadenopathy (59%) (Table 2). Reported rectal symptoms included purulent or bloody stools (21%), rectal pain (22%), and rectal bleeding (10%). Among 291 persons with available information about their first symptoms, 58% reported at least one prodromal symptom††; for the 42% of patients without prodromal symptoms, illness began with a rash.
Rash was most frequently reported on the genitals (46%), arms (40%), face (38%), and legs (37%); among 718 persons with monkeypox who reported body regions with rash, 238 (33%) reported rash in one region, 126 (18%) in two regions, 98 (14%) in three regions, and 256 (36%) in four or more regions. Among 104 persons with information on the number of lesions, 88% of cases involved fewer than 50 lesions.
Among 334 persons with data available on HIV status, 136 (41%) had HIV infection. Among 954 persons with hospitalization data available, 77 (8%) patients were hospitalized because of their illness. No deaths were reported. Among 339 persons with vaccination status available, 48 (14%) reported previous receipt of smallpox vaccine, including 11 (23%) who received 1 of 2 JYNNEOS doses during the current outbreak, 11 (23%) who received pre-exposure prophylaxis at an unknown time before the current outbreak, and 26 (54%) who did not provide information about when vaccine was administered. Among the recently vaccinated persons with monkeypox, at least one experienced symptoms >3 weeks after their first JYNNEOS dose.
Discussion
Current findings indicate that community transmission of monkeypox is widespread and is disproportionately affecting gay, bisexual, and other men who have sex with men; this is consistent with data reported from other countries (3). Public health efforts to slow monkeypox transmission among gay, bisexual, and other men who have sex with men require addressing challenges that include homophobia, stigma, and discrimination. Although the largest proportion of cases have occurred in White persons, Black and Hispanic persons, who represent approximately one third (34%) of the general population (4), accounted for more than one half (54%) of monkeypox cases in persons for whom information on race and ethnicity is available; further, the proportion of cases among Black persons has increased during recent weeks.Ensuring equity in approaches to monkeypox testing, treatment, and prevention is critical, and taking actions to minimize stigma related to monkeypox can reduce barriers to seeking care and prevention. The data presented in this report provide insights into early transmission; however, ongoing surveillance is essential to monitor future transmission trends and assess the impacts among different communities.
These data can guide clinical considerations for evaluating persons for monkeypox. Typically, monkeypox begins with a febrile prodrome, which might include malaise, chills, headache, or lymphadenopathy, followed by a disseminated rash that often includes the palms and soles (5). Although most cases in this report included these features, 42% of persons did not report prodromal symptoms, and 37% did not report fever by the time of interview. Genital rash, although reported in fewer than one half of cases, was common; 36% of persons developed rash in four or more body regions.
Other recent reports describe similar clinical characteristics (6,7). Clinicians should be vigilant for patients with rash consistent with monkeypox, regardless of whether the rash is disseminated or was preceded by prodrome. Likewise, although most cases to date have occurred among gay, bisexual, and other men who have sex with men, any patient, regardless of sexual or gender identity, with rash consistent with monkeypox should be considered for testing because close physical contact with an infectious person or exposure to contaminated materials such as clothing or bedding can result in transmission.
A substantial proportion of monkeypox cases have been reported among persons with HIV infection, and efforts are underway to characterize monkeypox clinical outcomes among these persons. Recent reports have found that concurrent sexually transmitted infections were common in persons with monkeypox (3,7). Clinicians and health officials implementing monkeypox education, testing, and prevention efforts should also incorporate recommended interventions for other conditions occurring among gay and bisexual men, including HIV infection, sexually transmitted infections, substance use, and viral hepatitis§§ (8).
On May 23, 2022, CDC launched an emergency response for monkeypox. This response includes educating providers and the public, expanding laboratory testing, outlining prevention strategies, and promoting the use of medical countermeasures for treatment and postexposure prophylaxis. CDC is supporting state, tribal, local, and territorial health departments through guidance and technical assistance. Testing capacity was rapidly expanded through CDC’s Laboratory Response Network and commercial laboratories, with national capacity estimates of 80,000 tests per week by July 18.¶¶
Because of long-standing investments in medical countermeasures for potential smallpox events, licensed vaccines and therapeutics for monkeypox are held in the U.S. Department of Health and Human Services Strategic National Stockpile. A national vaccine strategy was developed to equitably expand vaccination in areas experiencing high numbers of monkeypox cases and contacts. Two vaccines are available in the United States.*** As of August 3, more than 1 million doses of JYNNEOS, a nonreplicating, live virus vaccine (https://www.fda.gov/media/131078/download) had been allocated to jurisdictions, and approximately 14,700 courses of oral tecovirimat (TPOXX) had been distributed to jurisdictions and providers.
The findings in this report are subject to at least three limitations. First, this analysis includes only 41% of U.S. monkeypox cases reported through July 22 and might not be representative of all cases. Jurisdictions with high numbers of cases without submitted case report forms were more racially and ethnically diverse according to U.S. Census Bureau data; therefore, persons from racial and ethnic minority groups might be more disproportionately affected than indicated by these data. Second, even on submitted case report forms, data for variables such as timing of vaccination, sexual behaviors, HIV status, reason for hospitalization, and whether cases were travel-associated were frequently missing; data might also not reflect symptoms or outcomes occurring after the interview. Finally, persons with monkeypox who have mild symptoms might be less likely to seek care or initiate testing and could be underrepresented in this analysis.
CDC is continually evaluating new evidence and tailoring response strategies as information on changing case demographics, clinical characteristics, transmission, and vaccine effectiveness become available. Public health efforts should prioritize gay, bisexual, and other men who have sex with men, who are currently disproportionately affected for prevention and testing, address equity, and minimize stigma, while maintaining vigilance for transmission in other populations. Clinicians should test persons with rash consistent with monkeypox, regardless of whether the rash is disseminated or was preceded by prodrome.
abby normal
insert appropriate adjective here
Monkeyox found at New Orleans high school (Sci High)
The Louisiana Department of Health has confirmed a staff member at New Orleans Charter Science and Math High School tested positive for monkeypox last week, according to Sci High’s Head of School Monique Cola.
The news comes in the first weeks of a new school year, and as schools continue, for the third year, dealing with the COVID-19 pandemic.
Cola alerted families to the case, which was confirmed by state health officials on Friday, in a school-wide email sent on Sunday. The U.S. Centers for Disease Control has categorized the risk of children acquiring the virus in a school setting as low. It is spread through bodily fluids and contacts with surfaces that have been touched by an infected person.
In the email, Cola explained that on Aug. 15, during the second week of school, a staff member displayed potential symptoms of the virus.
“Our school-based health clinic evaluated the individual and sent them for testing that morning,” Cola wrote to families, noting the staff member stayed home for the rest of the week and that school staff disinfected all areas occupied by the individual that day.
On Friday, Cola said the state notified the school that the staff member had indeed tested positive and the LDH began contact tracing.
“Because of close physical contact, the Louisiana Department of Health will notify anyone deemed close contact with this individual,” Cola wrote. “However, this will be limited due to the fast and thorough actions of our staff and school-based health clinic.”
In closing, Cola wrote there would be “no operational changes for our school program” this week and that any questions could be directed to the school’s clinic.
The case appears to be the first identified among faculty or students in a New Orleans public school since the outbreak of the disease was identified in the United States earlier this year. The NOLA Public Schools district did not respond to a request for comment.
It is unclear whether the school district or LDH will publicly report monkeypox cases among school staff and students as they have with COVID-19.
The Department of Health confirmed the first case of monkeypox in a Louisiana resident on July 7. Since then, nearly 75 percent of Louisiana’s 146 confirmed cases are in the southeast region of the state, which includes New Orleans and surrounding parishes.
The Department of Health states “people most commonly get monkeypox through close and sustained skin-to-skin contact, including but not limited to intimate and sexual contact.”
Officials say it can also be spread through bodily fluid either via direct contact with lesions or by touching objects that have been used by someone with the virus.
The New Orleans Health Department will be offering free vaccines on Bourbon Street on Wednesday in advance of Southern Decadence, one of the country’s largest LGBTQ festivals.
New Orleans Health Director Dr. Jennifer Avegno said the city is paying close attention to the event and working to provide additional resources.
“Right now we do know that the majority of cases, both in Louisiana and around the country, are primarily in men who have sex with men and especially with multiple sexual partners,” Avegno told WWNO in an interview. “And that is a very large demographic of who’s going to be at Decadence.”

 thelensnola.org
thelensnola.org
The Louisiana Department of Health has confirmed a staff member at New Orleans Charter Science and Math High School tested positive for monkeypox last week, according to Sci High’s Head of School Monique Cola.
The news comes in the first weeks of a new school year, and as schools continue, for the third year, dealing with the COVID-19 pandemic.
Cola alerted families to the case, which was confirmed by state health officials on Friday, in a school-wide email sent on Sunday. The U.S. Centers for Disease Control has categorized the risk of children acquiring the virus in a school setting as low. It is spread through bodily fluids and contacts with surfaces that have been touched by an infected person.
In the email, Cola explained that on Aug. 15, during the second week of school, a staff member displayed potential symptoms of the virus.
“Our school-based health clinic evaluated the individual and sent them for testing that morning,” Cola wrote to families, noting the staff member stayed home for the rest of the week and that school staff disinfected all areas occupied by the individual that day.
On Friday, Cola said the state notified the school that the staff member had indeed tested positive and the LDH began contact tracing.
“Because of close physical contact, the Louisiana Department of Health will notify anyone deemed close contact with this individual,” Cola wrote. “However, this will be limited due to the fast and thorough actions of our staff and school-based health clinic.”
In closing, Cola wrote there would be “no operational changes for our school program” this week and that any questions could be directed to the school’s clinic.
The case appears to be the first identified among faculty or students in a New Orleans public school since the outbreak of the disease was identified in the United States earlier this year. The NOLA Public Schools district did not respond to a request for comment.
It is unclear whether the school district or LDH will publicly report monkeypox cases among school staff and students as they have with COVID-19.
The Department of Health confirmed the first case of monkeypox in a Louisiana resident on July 7. Since then, nearly 75 percent of Louisiana’s 146 confirmed cases are in the southeast region of the state, which includes New Orleans and surrounding parishes.
The Department of Health states “people most commonly get monkeypox through close and sustained skin-to-skin contact, including but not limited to intimate and sexual contact.”
Officials say it can also be spread through bodily fluid either via direct contact with lesions or by touching objects that have been used by someone with the virus.
The New Orleans Health Department will be offering free vaccines on Bourbon Street on Wednesday in advance of Southern Decadence, one of the country’s largest LGBTQ festivals.
New Orleans Health Director Dr. Jennifer Avegno said the city is paying close attention to the event and working to provide additional resources.
“Right now we do know that the majority of cases, both in Louisiana and around the country, are primarily in men who have sex with men and especially with multiple sexual partners,” Avegno told WWNO in an interview. “And that is a very large demographic of who’s going to be at Decadence.”

Monkeypox case confirmed at Sci High | The Lens
CDC says risk of in-school transmission is low.
psychgirl
Has No Life - Lives on TB
Here, we go.Monkeyox found at New Orleans high school (Sci High)
The Louisiana Department of Health has confirmed a staff member at New Orleans Charter Science and Math High School tested positive for monkeypox last week, according to Sci High’s Head of School Monique Cola.
The news comes in the first weeks of a new school year, and as schools continue, for the third year, dealing with the COVID-19 pandemic.
Cola alerted families to the case, which was confirmed by state health officials on Friday, in a school-wide email sent on Sunday. The U.S. Centers for Disease Control has categorized the risk of children acquiring the virus in a school setting as low. It is spread through bodily fluids and contacts with surfaces that have been touched by an infected person.
In the email, Cola explained that on Aug. 15, during the second week of school, a staff member displayed potential symptoms of the virus.
“Our school-based health clinic evaluated the individual and sent them for testing that morning,” Cola wrote to families, noting the staff member stayed home for the rest of the week and that school staff disinfected all areas occupied by the individual that day.
On Friday, Cola said the state notified the school that the staff member had indeed tested positive and the LDH began contact tracing.
“Because of close physical contact, the Louisiana Department of Health will notify anyone deemed close contact with this individual,” Cola wrote. “However, this will be limited due to the fast and thorough actions of our staff and school-based health clinic.”
In closing, Cola wrote there would be “no operational changes for our school program” this week and that any questions could be directed to the school’s clinic.
The case appears to be the first identified among faculty or students in a New Orleans public school since the outbreak of the disease was identified in the United States earlier this year. The NOLA Public Schools district did not respond to a request for comment.
It is unclear whether the school district or LDH will publicly report monkeypox cases among school staff and students as they have with COVID-19.
The Department of Health confirmed the first case of monkeypox in a Louisiana resident on July 7. Since then, nearly 75 percent of Louisiana’s 146 confirmed cases are in the southeast region of the state, which includes New Orleans and surrounding parishes.
The Department of Health states “people most commonly get monkeypox through close and sustained skin-to-skin contact, including but not limited to intimate and sexual contact.”
Officials say it can also be spread through bodily fluid either via direct contact with lesions or by touching objects that have been used by someone with the virus.
The New Orleans Health Department will be offering free vaccines on Bourbon Street on Wednesday in advance of Southern Decadence, one of the country’s largest LGBTQ festivals.
New Orleans Health Director Dr. Jennifer Avegno said the city is paying close attention to the event and working to provide additional resources.
“Right now we do know that the majority of cases, both in Louisiana and around the country, are primarily in men who have sex with men and especially with multiple sexual partners,” Avegno told WWNO in an interview. “And that is a very large demographic of who’s going to be at Decadence.”

Monkeypox case confirmed at Sci High | The Lens
CDC says risk of in-school transmission is low.thelensnola.org
Schools.
phloydius
Veteran Member
phloydius
Veteran Member
Okay, so this is very interesting. I quoted part of the article below. First, the bold is my emphasis, and is probably a typo, it probably was suppose to read that the "CDC determined through testing that it was a false positive."
Second, if I read the article right, that a PCR test was done and came back positive, and then the sample was sent to the CDC for testing and it came back as negative. My understanding is that the PCR test only tests for a orthopox virus (any orthopox virus) and the test that the CDC does is specifically for the "Orthopox MPXV". Thus someone could test positive for cowpox (Orthopox CPX) or smallpox (Orthopox VARV) on the PCR test and be told they have Monkeypox, and the CDC's test would come back negative.
So, maybe this child had cowpox or smallpox?

-------------
HOUSTON – Harris County Judge Lina Hidalgo provided an update on the monkeypox response and vaccination efforts Tuesday morning.
Hidalgo announced that health officials have learned that a child under 2 years old who was previously presumed positive for monkeypox did not have the virus and the CDC determined through testing that it was a false negative. The county judge said false positives can have 4% of the time.
“False positives do happen, they’re very rare,” Hidalgo said. “We haven’t had a false positive, this is the first one we’ve had with monkeypox of all the samples we’ve sent to the CDC. They all came back that in fact, that it was a positive, but this time, they came back and said that in fact, this case was a negative.”
Last edited:
psychgirl
Has No Life - Lives on TB
The information is out there, why this incessant need to lie, is beyond me!Has not spread to the kids yet. Ok, this is fine. The flame is way back by the tail of the Hindenburg, so nothing to worry about yet.
So, which is it? False POSITIVE, or false NEGATIVE?!! A bit of difference, there! Damn, I miss educated writers who actually proofread their work!Okay, so this is very interesting. I quoted part of the article below. First, the bold is my emphasis, and is probably a typo, it probably was suppose to read that the "CDC determined through testing that it was a false positive."
Second, if I read the article right, that a PCR test was done and came back positive, and then the sample was sent to the CDC for testing and it came back as negative. My understanding is that the PCR test only tests for a orthopox virus (any orthopox virus) and the test that the CDC does is specifically for the "Orthopox MPXV". Thus someone could test positive for cowpox (Orthopox CPX) or smallpox (Orthopox VARV) on the PCR test and be told they have Monkeypox, and the CDC's test would come back negative.
So, maybe this child had cowpox or smallpox?
-------------
HOUSTON – Harris County Judge Lina Hidalgo provided an update on the monkeypox response and vaccination efforts Tuesday morning.
Hidalgo announced that health officials have learned that a child under 2 years old who was previously presumed positive for monkeypox did not have the virus and the CDC determined through testing that it was a false negative. The county judge said false positives can have 4% of the time.
“False positives do happen, they’re very rare,” Hidalgo said. “We haven’t had a false positive, this is the first one we’ve had with monkeypox of all the samples we’ve sent to the CDC. They all came back that in fact, that it was a positive, but this time, they came back and said that in fact, this case was a negative.”
Summerthyme
why this incessant need to lie, is beyond me!
It's who they are.
Please read People of the Lie: The Hope for Healing... book by M. Scott Peck
bw
Fringe Ranger
I don't think immediate count updates are a good idea. Once a day should do, and once a week would give a better grasp of the situation. I suggest choosing a time of day to get the official count, and perhaps give a little context. Comparing to same time yesterday and last week, maybe. My 2p.
SouthernBreeze
Has No Life - Lives on TB
I don't think immediate count updates are a good idea. Once a day should do, and once a week would give a better grasp of the situation. I suggest choosing a time of day to get the official count, and perhaps give a little context. Comparing to same time yesterday and last week, maybe. My 2p.
I agree. An overall view would be better along with some context.
psychgirl
Has No Life - Lives on TB
I do it this way, on some days, to show how fast cases are rising on that particular day.I don't think immediate count updates are a good idea. Once a day should do, and once a week would give a better grasp of the situation. I suggest choosing a time of day to get the official count, and perhaps give a little context. Comparing to same time yesterday and last week, maybe. My 2p.
But whatever.
abby normal
insert appropriate adjective here
"YET"
Almost like they know something

bw
Fringe Ranger
I totally applaud your efforts. How about choosing one update time and call that the start count for the day. Then each time you post the newest count you might paste in the start count and maybe the one from yesterday? Just a thought.I do it this way, on some days, to show how fast cases are rising on that particular day.
Believe me, I don't want to discourage you!
SouthernBreeze
Has No Life - Lives on TB
It's probably impossible to get this info, but what I'd like to see are charts giving the breakdown of all these cases. What percentage are gay men? What percentage are women? What percentage are children? etc......Just number of cases give only a general idea of what's actually going on. Also, a daily count and a weekly count would be good, too.
Not trying to discourage anyone, cause like I said, this info might not be available, but it's what I was meaning by "context".
Not trying to discourage anyone, cause like I said, this info might not be available, but it's what I was meaning by "context".
Kayak
Adrenaline Junkie
There are plenty of gender charts out there showing that 99% of those testing positive are men, and the other one percent are also men (but identify as women) -- however, in those areas they are only testing gay men, so that information is exactly what you'd expect, and completely worthless.It's probably impossible to get this info, but what I'd like to see are charts giving the breakdown of all these cases. What percentage are gay men? What percentage are women? What percentage are children? etc......Just number of cases give only a general idea of what's actually going on. Also, a daily count and a weekly count would be good, too.
Not trying to discourage anyone, cause like I said, this info might not be available, but it's what I was meaning by "context".
SouthernBreeze
Has No Life - Lives on TB
There are plenty of gender charts out there showing that 99% of those testing positive are men, and the other one percent are also men (but identify as women) -- however, in those areas they are only testing gay men, so that information is exactly what you'd expect, and completely worthless.
Then the info I'm looking for is unavailable. I would consider it highly useful if it were.
Based on what I understand you to be saying is that out of the 44,063 cases to date, 99% of those are gay men. Correct?
Last edited:
abby normal
insert appropriate adjective here
HCLHD investigates Monkeypox case at Texas State
SAN MARCOS — An individual in the Texas State University community has tested positive for Monkeypox.
Dr. Emilio Carranco, Chief Medical Officer and Director of the Student Health Center, sent an emergency notification email to the Texas State faculty, staff and students in the morning hours of Tuesday, Aug. 23, to inform them of the situation.
The individual lives off campus and will remain in isolation until the rash heals and is no longer contagious as recommended by CDC guidelines, according to the email. The Hays County Local Health Department (HCLHD) will conduct a case investigation and assist in identifying and contacting close contacts of the positive case.
“While the risk of exposure to Texas State campuses remains low, this notice is being sent to comply with requirements of the Clery Act,” Carranco said in the email. “The university will carefully analyze any subsequent or additional Monkeypox reports on a case-by-case basis and will issue additional notices only if other significant factors warrant such notification.”
To prevent Monkeypox infection and spreading to others, the university community is encouraged to take the following steps:
- Avoid skin-to-skin contact with a person who has developed a pimple or blister-like rash
- Do not share utensils or touch bedding, clothing or towels used by a person with monkeypox
- Wash your hands often with soap and water or use hand sanitizer
- Watch for monkeypox symptoms such as muscle aches, fatigue, headache, fever, swollen lymph nodes, sore throat, congestion, or cough
- Watch for a new pimple or blister-like rash in the genital area, chest, arms, hands, or face
- If you suspect monkeypox, wear a face mask, isolate from others, and call your primary care provider or the Student Health Center at 512-245-2161 to schedule an evaluation
- Information on Monkeypox is available on the Texas State Student Health Center website.

HCLHD investigates Monkeypox case at Texas State
Staff Report SAN MARCOS -- An individual in the Texas State University community has tested positive for Monkeypox. Dr. Emilio Carranco, Chief Medical Officer and Director of the Student Health Center, sent an emergency notification... #DrEmilioCarranco #HaysCounty #HaysCountyLocalHealthDepartment
Kayak
Adrenaline Junkie
Then the info I'm looking for is unavailable. I would consider it highly useful if it were.
A while back, one of the European nations was testing everyone and posting gender info, and it was 60 something percent men and the rest women. I didn't make a note of which country, and I can't find anyone still doing so.
But yes, it feels as if this is information we need, which means TPTB aren't likely to give it to us when it doesn't support their narrative that this is just a gay disease.
Shadow
Swift, Silent,...Sleepy
Great phraseology! They have admitted to it being in a very few schools. Four weeks from now we will see what will happen when children share.Has not spread to the kids yet. Ok, this is fine. The flame is way back by the tail of the Hindenburg, so nothing to worry about yet.
Shadow
SouthernBreeze
Has No Life - Lives on TB
Great phraseology! They have admitted to it being in a very few schools. Four weeks from now we will see what will happen when children share.
Shadow
That is exactly what I'm waiting to see. What will it do is the big question.
Shadow
Swift, Silent,...Sleepy
There is a forum called FluTrackers which, oddly enough, tracks flu. But also tracks many others world wide. The monkeypox information seems to be by country rather than the whole world, but they tend to vet their information.Then the info I'm looking for is unavailable. I would consider it highly useful if it were.
Based on what I understand you to be saying is that out of the 44,063 cases to date, 99% of those are gay men. Correct?
The US page is. United States: monkeypox - FluTrackers News and Information
Shadow
psychgirl
Has No Life - Lives on TB
They’re very good.There is a forum called FluTrackers which, oddly enough, tracks flu. But also tracks many others world wide. The monkeypox information seems to be by country rather than the whole world, but they tend to vet their information.
The US page is. United States: monkeypox - FluTrackers News and Information
Shadow
Well respected. I used to follow them
bw
Fringe Ranger
That's what the testing shows. So if it's out on the loose in the hetero community, which seems an increasingly unavoidable conclusion, then the actual infections is not merely some multiple of the test results, but a multiple of THAT estimate.Based on what I understand you to be saying is that out of the 44,063 cases to date, 99% of those are gay men. Correct?
bw
Fringe Ranger
When they're ready to move the herd, the tell will be in their dropping the 'gay disease' trope.when it doesn't support their narrative that this is just a gay disease.
SouthernBreeze
Has No Life - Lives on TB
That's what the testing shows. So if it's out on the loose in the hetero community, which seems an increasingly unavoidable conclusion, then the actual infections is not merely some multiple of the test results, but a multiple of THAT estimate.
In my mind, the jury is still out on that. We're still not seeing widespread cases outside of the gay community whether they're being tested or not. Of course, that's just my opinion. I understand if others don't agree.
Meemur
Voice on the Prairie / FJB!
In my mind, the jury is still out on that. We're still not seeing widespread cases outside of the gay community whether they're being tested or not. Of course, that's just my opinion. I understand if others don't agree.
I'm waiting until the end of September to make up my mind.
psychgirl
Has No Life - Lives on TB
bw
Fringe Ranger
Depending on when those women came into the system, that might be one hetero guard. How many more have not yet tested positive?Prison cases
psychgirl
Has No Life - Lives on TB
Who knows.Depending on when those women came into the system, that might be one hetero guard. How many more have not yet tested positive?
phloydius
Veteran Member
Based on what I understand you to be saying is that out of the 44,063 cases to date, 99% of those are gay men. Correct?
What you'll find is in the official reports they will use words like "of cases with available data" which will be left off the numbers reported in the media. The dataset that the WHO has is what is quoted by the CDC, media, doctors, and pretty much everyone else.
As of 23rd August, the WHO is still reporting only 41,664 cases & reports that 98.2% of cases with available data are male. The WHO states they know that 20,138 are known to be males, 362 are known to be females, and they do not know the sex of 21,164 cases.
When they report age, they only know the age of 23,626 cases.
A number you'll see reported often is that it is "99% gay men". The current number is now 95.8% are gay men (technically men who have sex with men, because it also includes bisexuals). However, that 95.8% is only based on 9,899 cases. They do not know the sexual orientation of 31,765 of the 41,664 cases!
Now, of course logically the percentages of gender and sexual orientation probably are similar in the "unknown" cases as well, if all things are equal. Although if (as just an example), the people tested at a sexual health clinic are asked about sexual orientation but people at a GP (Primary Care Doctor) or the ER are not, then the numbers could be off quite a bit.
