You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
CORONA Main Coronavirus thread
- Thread starter Heliobas Disciple
- Start date
-
- Tags
- coronavirus
jward
passin' thru
Craig Kelly
@CraigKellyPHON
OXFORD’S CORRUPTED IVERMECTIN STUDY FINALLY PUBLISHED.
They tried their best, but they couldn‘t mask the effectiveness of Ivermectin against Covid.
 They failed to combine the Ivermectin with Zinc & Doxycycline - when they knew it was this combination that was being recommended in all published Ivermectin protocols
They failed to combine the Ivermectin with Zinc & Doxycycline - when they knew it was this combination that was being recommended in all published Ivermectin protocols
 They delayed the start of treatment, enrolling patients in the trial up to 14 days after the onset of symptoms - when they knew that extensive research shows that early antiviral treatment is critical and the published protocols call for treatment to be started "immediately" after first symptoms.
They delayed the start of treatment, enrolling patients in the trial up to 14 days after the onset of symptoms - when they knew that extensive research shows that early antiviral treatment is critical and the published protocols call for treatment to be started "immediately" after first symptoms.
 They told patients to take Ivermectin on an empty stomach - when they should have known that the published science shows this significantly diminishes its effectiveness and that all the published protocols recommend Ivermectin be taken with food.
They told patients to take Ivermectin on an empty stomach - when they should have known that the published science shows this significantly diminishes its effectiveness and that all the published protocols recommend Ivermectin be taken with food.
 They only administered the Ivermectin for just 3 days - when the published protocols call for it be administered for 5 days and extended to 30 days in case of continued symptoms.
They only administered the Ivermectin for just 3 days - when the published protocols call for it be administered for 5 days and extended to 30 days in case of continued symptoms.
And yet despite these tricks and many others, they still couldn’t hide Ivermectin’s effectiveness, with their results showing those taking Ivermectin had a
 28% improvement in recovery at 3, 6 & 12 months
28% improvement in recovery at 3, 6 & 12 months
 23% improvement in an early sustained recovery
23% improvement in an early sustained recovery
 23% improvement in reducing muscle ache
23% improvement in reducing muscle ache
 22% improvement in reducing Fever
22% improvement in reducing Fever
 21% improvement in alleviating headaches
21% improvement in alleviating headaches
 17% improvement in alleviating abdominal pain
17% improvement in alleviating abdominal pain
 16% improvement in alleviating coughs
16% improvement in alleviating coughs
 16% improvement in the alleviation of all symptoms
16% improvement in the alleviation of all symptoms
 13% improvement in first reported recovery
13% improvement in first reported recovery
And further, patients in the ivermectin group were also found to had significantly better health one year later.
We are only left to speculate how much more improvement would have occurred if this corrupted trial started treatment immediately, extended treatment beyond the 3 days and combined the Ivermectin with Zinc & Doxycycline (and Vitamin D, and Betadine gargles)
Yet bizarrely (but not unexpected given this study was designed to fail) the authors conclude nothing to see here and give a conclusion that is contrary to evidence found.
But as always follow the money - there’s a $100 billion market in Ivermectin’s patented Big Pharma competitors ; Molnupirvir and Paxlovid. And if the truth is acknowledged about Ivermectin its all over for Molnupirvir and Paxlovid.
To design and carry out a medical study designed to fail is a crime against humanity. The authors of this study should be amongst the first in the docks at Nuremberg 2.0
The effectiveness of Ivermectin is only further confirmed by this study.
Further reading : PRINCIPLE: significantly improved recovery and lower long COVID with ivermectin
Study : https://sciencedirect.com/science/articl
View: https://twitter.com/CraigKellyPHON/status/1763897967537467535?s=20
@CraigKellyPHON
OXFORD’S CORRUPTED IVERMECTIN STUDY FINALLY PUBLISHED.
They tried their best, but they couldn‘t mask the effectiveness of Ivermectin against Covid.
And yet despite these tricks and many others, they still couldn’t hide Ivermectin’s effectiveness, with their results showing those taking Ivermectin had a
And further, patients in the ivermectin group were also found to had significantly better health one year later.
We are only left to speculate how much more improvement would have occurred if this corrupted trial started treatment immediately, extended treatment beyond the 3 days and combined the Ivermectin with Zinc & Doxycycline (and Vitamin D, and Betadine gargles)
Yet bizarrely (but not unexpected given this study was designed to fail) the authors conclude nothing to see here and give a conclusion that is contrary to evidence found.
But as always follow the money - there’s a $100 billion market in Ivermectin’s patented Big Pharma competitors ; Molnupirvir and Paxlovid. And if the truth is acknowledged about Ivermectin its all over for Molnupirvir and Paxlovid.
To design and carry out a medical study designed to fail is a crime against humanity. The authors of this study should be amongst the first in the docks at Nuremberg 2.0
The effectiveness of Ivermectin is only further confirmed by this study.
Further reading : PRINCIPLE: significantly improved recovery and lower long COVID with ivermectin
Study : https://sciencedirect.com/science/articl
View: https://twitter.com/CraigKellyPHON/status/1763897967537467535?s=20
Heliobas Disciple
TB Fanatic
World’s First Tissue Bank Could Solve Mystery of Long COVID Misery
UC San Francisco is set to launch the world’s first tissue bank with samples donated by patients with long COVID. The move follows research indicating that the virus can continue to linger throughout the body and may hold the key to understanding the cause of the debilitating disorder, leading to ef
scitechdaily.com
World’s First Tissue Bank Could Solve Mystery of Long COVID Misery
By University of California - San Francisco
March 1, 2024
UC San Francisco is set to launch the world’s first tissue bank with samples donated by patients with long COVID. The move follows research indicating that the virus can continue to linger throughout the body and may hold the key to understanding the cause of the debilitating disorder, leading to effective treatments.
By October 2023, an estimated 14% of Americans had or had had long COVID, according to the Centers for Disease Control and Prevention. The disorder may appear as a continuation of the original COVID symptoms or manifest as new symptoms affecting any part of the body. In serious cases, multiple body systems are affected, including the brain, heart, lungs, kidneys, and skin.
Recent studies have shown that in patients with long COVID, the SARS-CoV-2 virus may not fully clear after the initial infection. Instead, the virus remains in what scientists have termed “viral reservoirs,” identified in patient tissue months or even years later. These reservoirs are now believed to be a primary driver of long COVID, provoking the immune system to respond by prompting conditions like blood clotting disorders, inflammation, and cognitive dysfunction.
“Based on our work so far, we believe that long COVID is a tissue-based disease,” said Michael Peluso, MD, principal investigator of the UCSF Long COVID Tissue Program and an infectious disease physician-scientist in the UCSF School of Medicine.
“This program will allow us to comprehensively study the biological processes occurring across tissue compartments – in the blood, gut, lymph nodes, spinal fluid, and bone marrow – in people living with long COVID. This will help us better understand the underlying mechanisms of long COVID,” said Peluso, who co-led recent research with Timothy Henrich, MD, a UCSF physician-scientist, that showed the virus was present in colon tissue up to 676 days following infection.
An effort to expand collaboration with HIV/AIDS, cardiology, and other specialists
Tissue specimens will be acquired from existing and future participants enrolled in UCSF’s LIINC study, and shared with non-UCSF scientists conducting complementary research. The study, which was launched in April 2020 before long COVID was recognized, is open to all adults who have ever tested positive for COVID-19.
“The persistence of SARS-CoV-2 in tissue is a major target for our rapid research and clinical trials,” said Steven Deeks, MD, co-principal investigator of LIINC, professor of medicine in residence at UCSF and an internationally recognized HIV expert. Current clinical trials include a monoclonal antibody – a lab-made protein that effectively attacks viruses – and an antiviral therapy that blocks viral replication.
The UCSF Long COVID Tissue Program is supported by a $3 million grant from the Long Covid Research Consortium of the PolyBio Research Foundation, a nonprofit dedicated to complex chronic conditions, which also funded the LIINC study.
“The UCSF team includes people who helped make HIV and AIDS a treatable disease,” said Amy Proal, PhD, president of PolyBio. “These researchers rapidly pivoted into long COVID research at the outset of the pandemic, leveraging years of experience performing similar research with patients with HIV and AIDS.”
An additional $1.7 million funding from PolyBio will also enable Henrich, and UCSF cardiologist Zian Tseng, MD, to expand their study of sudden cardiac death. Advanced technologies will be used to examine traces of SARS-CoV-2 and related immune changes in tissue samples. Findings may result in recommendations for antiviral treatments for patients who have been exposed to the COVID virus and are at risk for sudden cardiac death.
Reference: “Multimodal Molecular Imaging Reveals Tissue-Based T Cell Activation and Viral RNA Persistence for Up to 2 Years Following COVID-19” by Michael J. Peluso, Dylan Ryder, Robert Flavell, Yingbing Wang, Jelena Levi, Brian H. LaFranchi, Tyler-Marie Deveau, Amanda M. Buck, Sadie E. Munter, Kofi A. Asare, Maya Aslam, Wally Koch, Gyula Szabo, Rebecca Hoh, Monika Deswal, Antonio Rodriguez, Melissa Buitrago, Viva Tai, Uttam Shrestha, Scott Lu, Sarah A. Goldberg, Thomas Dalhuisen, Matthew S. Durstenfeld, Priscilla Y. Hsue, J. Daniel Kelly, Nitasha Kumar, Jeffrey N. Martin, Aruna Gambir, Ma Somsouk, Youngho Seo, Steven G. Deeks, Zoltan G. Laszik, Henry F. VanBrocklin and Timothy J. Henrich, 31 July 2023, medRxiv.
DOI: 10.1101/2023.07.27.23293177
Heliobas Disciple
TB Fanatic

COVID-19 rapid tests still work against new variants—researchers keep 'testing the tests,' and they pass
By September 2020, just six months after COVID-19 triggered shutdowns across the U.S., it was clear that SARS-CoV-2, the virus that causes COVID-19, had mutated from its original form.
COVID-19 rapid tests still work against new variants—researchers keep 'testing the tests,' and they pass
by Nathaniel Hafer, Anuradha Rao and Apurv Soni, The Conversation
March 2, 2024
By September 2020, just six months after COVID-19 triggered shutdowns across the U.S., it was clear that SARS-CoV-2, the virus that causes COVID-19, had mutated from its original form.
The question quickly arose whether existing rapid antigen tests could detect newly emerging variants.
Using clinical samples obtained from diagnostic labs throughout the U.S. from 2020 to 2023, the National Institutes of Health, through its Variant Task Force, analyzed the effectiveness of more than 100 rapid antigen test kits on over 300 variants. The vast majority of the kits were able to detect new as well as prior previously known variants.
We are a team of researchers who have spent the past few years researching COVID-19 tests for their accuracy and performance. We understand why the public may still have questions about whether these tests are reliable, particularly as new variants continue to appear.
Here are answers to some of those questions:
Do these tests work?
There are two major types of tests for the detection of SARS-CoV-2.
The first, called a RT-PCR test, is more than 95% accurate for detecting the virus. These were the tests that most Americans were given at drive-through and walk-in testing sites early in the pandemic. The vast majority are now done at a doctor's office or clinic, though there are some home PCR tests, which typically cost five to 10 times more than rapid antigen tests.
The other type is an antigen test, commonly known as a rapid test, with an accuracy rate of more than 80%. Most of these tests are sold over the counter at supermarkets and pharmacies.
Rapid antigen tests are relatively inexpensive, can be used without prior training and give quick results, typically within 10 or 15 minutes. One drawback is that they are less accurate than PCR tests, especially early in an infection when there is less virus present in the body.
Despite these inherent limitations, our team has demonstrated that these tests perform as well in 2024 as they did earlier in the pandemic, when different variants were circulating—even though our initial study was completed in January 2022. That's because the virus protein detected by antigen tests has not changed much over the last two years, unlike other parts of the virus that have undergone many mutations. Another study, which tested the accuracy of rapid antigen tests from 2020 to 2022, found similar results.
That said, researchers like us continue to "test the tests," both in computer simulations and in the lab, to detect new SARS-CoV-2 variants.
I have symptoms. When should I take a test?
If you have symptoms, take a rapid test as soon as possible. If you test positive, you can be reasonably certain that you're infected. If you're negative, wait two days and test again.
This waiting period is important because it takes a few days for the virus to build up to levels that are detectable by the rapid test. Recent research has shown that the time it takes for this to happen is slightly longer with the omicron family of variants compared to variants from a few years ago.
I was exposed, but have no symptoms. When do I test?
If you've been exposed to somebody but don't have symptoms, the current recommendation is to wait four to five days before taking a rapid test. If you're negative, wait two days and then test again.
If you're still negative, take a third test two more days later. This is the best way to detect COVID-19 infection without symptoms.
It's also recommended that you take a rapid test as close as possible to the time you're visiting someone who is at risk for getting sick, especially if you think you may have been exposed.
When am I contagious?
Most people who have symptoms and test positive are contagious. If you no longer have symptoms and are no longer testing positive, it's likely that you're not contagious.
But there are some exceptions to this general rule. It's possible to be infected, have no symptoms and be contagious. This is especially true early on in a person's infection.
Should I swab my nose or throat?
The best advice is to follow the instructions that come with your test. For antigen tests in the U.S., this means taking a swab of your nose.
Although one study from Denmark reported that antigen tests were more sensitive when a health care provider swabbed the throat, the same study said that when a person swabbed themselves, nose samples were more accurate than throat samples. Other studies have shown that swabbing the throat was no better than swabbing the nose.
A new program funded by the National Institutes of Health and rolled out in late 2023—the Home Test to Treat study—offers free testing, telehealth and treatment for COVID-19 and the flu without leaving home. To date, more than 60,000 people have enrolled. The study uses commercially available rapid tests and typically arrive a few days after they're requested.
For those millions of Americans who are unable to travel, are without insurance, don't live near a clinic or simply don't want to expose others to their symptoms, this new program could help save lives.
Heliobas Disciple
TB Fanatic
Loading…
www.thailandmedical.news
Doctors Warn That COVID-19 Infections Can Cause Spontaneous Tears (Dissections) In The Walls Of The Coronary Artery
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 03, 2024
The COVID-19 pandemic, caused by the SARS-CoV-2 virus, has not only ravaged the respiratory system but has also left an indelible mark on the cardiovascular system. While the cardiovascular implications of COVID-19 have been extensively studied, a lesser-explored realm is the potential link between COVID-19 and Spontaneous Coronary Artery Dissection (SCAD). SCAD, characterized by a tear in the coronary artery wall, poses a unique threat as it can lead to heart attacks or even cardiac arrest. This COVID-19 News report delves into the intricate relationship between COVID-19 and SCAD, combining insights from studies conducted at the University Hospital of Patras-Greece, Hippocration General Hospital, and the National and Kapodistrian University of Athens-Greece.
Thailand Medical News would like to add that a number of case reports and studies have also validated that SARS-CoV-2 infections can cause these spontaneous tears in the walls of the coronary artery which can lead to heart attacks and also fatal outcomes.
https://journals.sagepub.com/doi/10.1177/2050313X20975989
https://journal.chestnet.org/article/S0012-3692(22)01575-6/fulltext
COVID-19 and spontaneous coronary artery dissection: causality? | Scientific letter
https://onlinelibrary.wiley.com/doi/10.1002/ccr3.6399
https://www.sciencedirect.com/science/article/pii/S2589790X24000271
Spontaneous Coronary Artery Dissection as a Cause of Acute Myocardial Infarction in COVID-19 Patients: A Case Report and Review of the Literature
Spontaneous Coronary Artery Dissection (SCAD) in an Atypical Patient Without Risk Factors and Prior Asymptomatic COVID-19 Infection
Spontaneous coronary artery dissection: review, case report and analysis of COVID-19-related cases - Minerva Cardiology and Angiology 2023 Feb 27
https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/ru/covidwho-1995813
Spontaneous Coronary Artery Dissection Following SARS-CoV-2-Associated Multisystem Inflammatory Syndrome
Spontaneous Coronary Artery Dissection as a Cause of Acute Myocardial Infarction in COVID-19 Patients: A Case Report and Review of the Literature
Cardiovascular Manifestations of COVID-19
COVID-19's impact extends beyond the respiratory system, affecting the cardiovascular system through various mechanisms. The virus utilizes the angiotensin-converting enzyme 2 (ACE-2) receptor, causing endothelial dysfunction, hypercoagulability, and inflammation. Cardiovascular manifestations include acute coronary syndrome, arrhythmias, cardiogenic shock, and cardiomyopathy. The interplay of systemic inflammation, direct viral effects on myocardial cells, and vascular infection increases the risk of myocardial infarction. Notably, macrophages and foam cells within plaques are susceptible to SARS-CoV-2 infection, leading to inflammation and plaque destabilization.
Understanding Spontaneous Coronary Artery Dissection (SCAD)
SCAD emerges as a rare manifestation of coronary artery disease, with up to 4% of acute coronary syndrome (ACS) patients experiencing it. More prevalent in females, SCAD often occurs without typical cardiovascular risk factors, affecting individuals between 44 to 53 years old. Predisposing factors include pregnancy, contraceptive pill use, hypertension, dyslipidemia, arteriopathies, connective tissue disorders, and emotional or physical stressors.
Pathophysiology of SCAD
SCAD, a non-traumatic rupture of the coronary wall, leads to acute coronary syndrome and sudden death. Two main hypotheses, "inside-out" and "outside-in," explain blood entry into the sub-intimal space or de novo intramural hematoma formation. Inflammation and connective tissue abnormalities contribute to SCAD pathophysiology. Autopsy reports reveal an inflammatory infiltrate in the outer connective tissue layer of affected coronary arteries.
Association of COVID-19 with SCAD: Possible Mechanisms
Several theories link COVID-19 to SCAD, suggesting a multifactorial process. Intense inflammation and endothelial dysfunction may cause sympathetic over-reactivity, leading to intimal dissection. SARS-CoV-2 infection induces T-cell infiltration, cytokine production, and protease release, increasing the risk of plaque rupture or erosion. Another mechanism involves angiogenesis stimulation and vasa vasorum proliferation, leading to intramural hematoma formation. Direct viral infection of coronary vessels can also weaken vessel walls, predisposing them to dissection.
Special Considerations and Case Reports
Male involvement in SCAD cases related to COVID-19 challenges the gender-specific trend seen in typical non-COVID-19 related SCAD. Symptoms vary, with chest pain being the most common, but some patients exhibit atypical symptoms. Diagnostic challenges highlight the need for advanced imaging techniques like intravascular ultrasound and optical coherence tomography. Management decisions, ranging from conservative pharmacotherapy to invasive interventions like percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG), depend on clinical presentation and risk assessment.
Discussion and Management Strategies
The complex association between COVID-19 and SCAD necessitates careful consideration of diagnostic and management strategies. The heightened risks associated with revascularization procedures in SCAD patients underscore the need for individualized treatment based on clinical presentation. The psychological impact of SCAD, exacerbated by pandemic-related stressors, emphasizes the importance of addressing mental health in recovery.
Conclusion
As the world grapples with the evolving challenges of the COVID-19 pandemic, understanding its impact on various organ systems, including the cardiovascular system, is crucial. The intricate relationship between COVID-19 and SCAD warrants further research to guide effective diagnostic and treatment approaches. This article aims to shed light on the complex interplay between these two entities, emphasizing the need for ongoing studies and collaboration within the medical community to enhance our understanding and improve patient outcomes.
The study findings were published in the peer reviewed journal: Life.

Spontaneous Coronary Artery Dissection and COVID-19: A Review of the Literature
SARS-CoV-2 is responsible for the global coronavirus disease 2019 (COVID-19) pandemic. While the cardiovascular effects of COVID-19 have been thoroughly described, there are limited published studies in the literature establishing a connection between spontaneous coronary artery dissection...
Heliobas Disciple
TB Fanatic
Embalmers’ Clots - How Can They Form Pre-mortem?
Vejon Health
Streamed live March 2, 2024
47 min 36 sec
What could be the scientific explanation for these observations of clots with embalmers and also in catheter labs?
Watch Embalmers Clots in the Living! Whistle-blower speaks.
Exploring the science.
Professor Resia Pretorius is a Physiologist, distinguished professor and Chair in the Department of Physiological Sciences, Stellenbosch University, South Africa. She studies cells and proteins in the coagulation system, including platelets, erythrocytes and the coagulation plasma protein, fibrin(ogen). She also studies inflammatory biomarkers, including those that have a viral and bacterial origin, that might impact on the coagulation system.
Dr. Robin Rose (Terrain Health), a board-certified specialist in gastroenterology and internal medicine. Focused on microclots in long covid patients.
Kell, Douglas B., Gert Jacobus Laubscher, and Etheresia Pretorius. "A central role for amyloid fibrin microclots in long COVID/PASC: origins and therapeutic implications." Biochemical Journal 479.4 (2022): 537-559.
Loading…
portlandpress.com
Latest news, research and updates about COVID-19 and health.
Alternative Links Here: Substack - COVID-19: Vejon COVID-19 Review | Dr Philip McMillan | Substack
Heliobas Disciple
TB Fanatic

New Study Challenges Conventional Wisdom on Lockdowns
New research highlights the fine balance between health and economic strategies in pandemic response, introducing an innovative approach that adapts to changing virus dynamics. The COVID-19 pandemic raised questions about when and to what extent costly nonpharmaceutical interventions (e.g., lockd
scitechdaily.com
New Study Challenges Conventional Wisdom on Lockdowns
By Carnegie Mellon University
March 3, 2024
New research highlights the fine balance between health and economic strategies in pandemic response, introducing an innovative approach that adapts to changing virus dynamics.
The COVID-19 pandemic raised questions about when and to what extent costly nonpharmaceutical interventions (e.g., lockdowns) should be used to slow the contagious spread of the virus. In a new study, researchers tackled that question with a dynamic optimization model. They found that small changes can tip the optimal response between very different approaches and identified an alternate approach that has previously not been recognized as effective.
The study was conducted by researchers at Carnegie Mellon University, the International Institute for Applied Systems Analysis, the University of Vienna, Vienna University of Technology, Tilburg University, and the Vienna Academy of Sciences. It is published in Theoretical Population Biology.
Economic Versus Health Strategies
“Some interventions to slow disease spread are cheap, but others disrupt economic, educational, and social activity,” notes Jonathan P. Caulkins, professor of operations research and public policy at Carnegie Mellon’s Heinz College, who coauthored the study. “The latter force governments to balance the health benefits of reduced infection and death against broader lockdown-induced societal costs.”
Previous models exploring the optimal lockdown strategy for countering pandemics like COVID-19 found that policymakers often face a stark choice: It may be optimal to lock down very aggressively to more or less avoid the epidemic (a “health strategy”) or it may be optimal to use lockdowns more sparingly to delay but not avoid most people getting infected (an “economic strategy”). That work also found that small changes in certain key parameters can flip the optimal strategy from one extreme to the other.
Advancements in the SIR Model
Researchers have long observed that a population exposed to an infection can be divided into three categories: susceptible (S), infected (I), and recovered (R), creating an SIR model. Past research has examined how to adjust lockdown intensity as an epidemic evolves. In this study, researchers extended that work by augmenting the standard SIR model to include the possibilities that a) the protective effects of vaccines can ebb over time, 2) the virus can mutate in ways that render past immunity less effective, and 3) the resulting re-infections are less deadly than infections of people with no immunity.
Here, researchers referred to these three additional features as novelties, and investigated the effects of adding each successively to the basic SIR model. They then added another feature: an inflow of infections even when no one in the focus population was infected (e.g., infection from abroad). The study also considered duration and stock of immunity and lockdown intensity.
The Role of Nonpharmaceutical Interventions
More aggressive efforts to use nonpharmaceutical interventions such as lockdowns lead to fewer infections, but also to greater economic and social burdens. For example, China’s zero-COVID policy resulted in an extended and painful lockdown, and in many countries that closed schools, students’ educational progress was harmed.
A recurring theme in the analysis, say the researchers, is the existence of break-even or tipping points. If a parameter describing the infection or infection countermeasure is above that critical value, it would be best to follow one strategy, but if that parameter turned out to be below that critical value, it might lead to a very different strategy. Among those key parameters is the valuation society places on avoiding a COVID-19-induced death relative to the value placed on the economic, social, and educational harms caused by locking down important parts of society.
It is important to acknowledge this issue because parameters reflect individuals’ or society’s values; they are not a scientific fact that can be measured objectively. As a result, two people who agree on all the scientific facts can nonetheless reasonably and intelligently prefer different COVID control strategies.
Dynamic and Alternate Solutions
Another theme is the existence of alternate optimal solutions that reflect fundamentally different strategies. By augmenting the standard SIR model to include the features assessed in this study, researchers identified a third type of solution that uses periods of stricter and less strict lockdowns to accompany recurring epidemic waves.
While the existence of recurrent waves of epidemics and lockdowns might at first glance be considered evidence of policy failure, it can in fact be the best way to respond to the realities of a virus that mutates or otherwise defeats previously acquired immunity. The authors also note that policies that would have been optimal for COVID-19 might not be optimal for the next pandemic if the virus causing the next pandemic is a little more contagious or a little less deadly or a little less prone to mutate.
Conclusion: A Call for Compromise and Flexibility
“Whatever policy is pursued, its implementation should perhaps be tempered by the knowledge that it won’t be the preferred or right policy for every individual, and that evolving understanding of that new virus’s idiosyncratic properties might require even experts to change their mind,” says Dieter Grass, guest research scholar at the International Institute for Applied Systems Analysis and lead author of the study. “Choices about epidemic-related policies should be seen as an exercise in compromise for the collective good, not a matter of mechanically deducing the one, true, evidence-based policy that all rational people must favor.”
Reference: “Riding the waves from epidemic to endemic: Viral mutations, immunological change and policy responses” by D. Grass, S. Wrzaczek, J.P. Caulkins, G. Feichtinger, R.F. Hartl, P.M. Kort, M. Kuhn, A. Prskawetz, M. Sanchez-Romero and A. Seidl, 3 February 2024, Theoretical Population Biology.
DOI: 10.1016/j.tpb.2024.02.002
Heliobas Disciple
TB Fanatic
(fair use applies)
Brazil’s Healthcare Doomed As COVID-19 Infections Rise Along With Dengue, Flu, RSV, Malaria, Zika, Measles, TB, HIV And Cholera Infections
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 04, 2024
As Brazil grapples with the relentless onslaught of the COVID-19 pandemic, recent data released by the Fiocruz InfoGripe Bulletin paints a grim picture of the country's healthcare system. The report, unveiled on February 29th, reveals a concerning surge in COVID-19 cases, with an alarming twist. Not only is the COVID-19 crisis escalating, but Brazil is also witnessing a simultaneous rise in infections of Dengue, Malaria, Measles, Tuberculosis (TB), Human Immunodeficiency Virus (HIV), and Cholera.
Local COVID-19 News coverages show that most hospitals and emergency rooms across Brazil are inundated with sick individuals and causing a near collapse of the country’s public healthcare infrastructure.
Worrisome Regional Trends
The bulletin identifies a significant increase in respiratory infections and pneumonia cases linked to COVID-19 across the Central-South regions of Brazil. The Southeast, Central-West, and South regions are particularly hard-hit, displaying clear indicators of an upswing in COVID-19-related respiratory distress. Disturbingly, most states in the Center-South exhibit this upward trajectory, hinting at a widespread and escalating health crisis.
The Northeastern states are not immune to the surge, with some displaying signs of increased SARS, albeit the infectious agent responsible remains unclear. In Bahia, however, there is a notable association with influenza A, commonly known as the flu virus. The scenario raises concerns about potential co-circulation of viruses, complicating the healthcare landscape further.
Expert Analysis and Recommendations
Marcelo Gomes, a researcher from the Scientific Computing Program and coordinator of InfoGripe, emphasizes the gravity of the situation. Gomes underscores the national concern, emphasizing the troublesome co-circulation of COVID-19 and Influenza A in several Central-South states. Despite COVID-19 causing a significantly higher number of hospitalizations than the flu, the simultaneous circulation of both viruses poses unprecedented challenges to the already strained healthcare infrastructure.
Gomes reiterates the importance of adhering to preventive measures, urging individuals with respiratory infection symptoms to stay at home and rest. For those compelled to venture outside, the use of appropriate masks, such as PFF2 or N95, is strongly advised to curb virus transmission, especially when visiting healthcare facilities.
National Overview of COVID-19
Examining both long-term (last six weeks) and short-term (last three weeks) trends, the report identifies an alarming growth in respiratory infections incidence and mortality associated with COVID-19. Over the last eight weeks, the impact of respiratory infections remains most pronounced among young children and the elderly, with COVID-19 disproportionately affecting those under two years old and individuals over 65.
The report highlights other respiratory viruses, such as Respiratory Syncytial Virus (RSV) and rhinovirus, as significant contributors to respiratory infections incidence in young children. However, the mortality rates for respiratory infections, particularly related to COVID-19, remain significantly higher in the elderly population.
Regional Breakdown of Respiratory Infection Increases
Eighteen states exhibit concerning signs of long-term respiratory infections growth, including Bahia, Ceará, Distrito Federal, Espírito Santo, Goiás, Maranhão, Mato Grosso, Mato Grosso do Sul, Minas Gerais, Pará, Paraíba, Paraná, Rio Grande do Sul, Rio de Janeiro, Roraima, Santa Catarina, Sergipe, and São Paulo.
Specifically related to respiratory infection cases due to COVID-19, the Federal District, Espírito Santo, Goiás, Minas Gerais, Mato Grosso, Mato Grosso do Sul, Paraná, Rio de Janeiro, Rio Grande do Sul, Santa Catarina, and São Paulo display an alarming increase.
In Bahia, Rio de Janeiro, Rio Grande do Sul, Santa Catarina, and São Paulo, there is evidence of increased respiratory infections caused by influenza A (flu). In some states like Ceará, Maranhão, Pará, Paraíba, and Roraima, the rise in respiratory infections is concentrated among children, with the responsible viral agent yet to be determined.
City-Specific Concerns
Seventeen capitals across Brazil are witnessing a surge in severe respiratory infection cases, including Aracaju (SE), Belém (PA), Boa Vista (RR), Campo Grande (MS), Cuiabá (MT), Curitiba (PR), Florianópolis (SC), Fortaleza (CE), Goiânia (GO), João Pessoa (PB), Maceió (AL), Porto Velho (RO), Rio de Janeiro (RJ), Salvador (BA), São Luís (MA), São Paulo (SP), and Vitória (ES).
Respiratory Virus Prevalence and Mortality
Over the past four epidemiological weeks, the prevalence among cases with positive results for respiratory viruses included influenza A (10.3%), influenza B (0.3%), RSV (10.8%), and Sars-CoV-2/Covid-19 (70.6%). Among deaths, these viruses were present in influenza A (2.5%), influenza B (0.6%), RSV (0.6%), and SARS-CoV-2/COVID-19 (92.5%).
In the epidemiological year 2024, 10,985 Respiratory infection cases have been reported, with 37.7% having a positive laboratory result for a respiratory virus. COVID-19 dominates, comprising 69.6% of positive cases. Despite ongoing investigations, the fluid nature of case notifications and laboratory result insertions necessitates ongoing updates.
SARS-CoV-2 Variants At Play In Brazil
Based on data collated by Thailand Medical News, the predominating SARS-CoV-2 sub-lineages circulating in Brazil at the moment are JN.2.5, JN.1.7, JN.1.1 and JN.1.
Dengue Rising at exponential rates in Brazil
Refer:
Conclusion
Brazil is facing a healthcare crisis of unprecedented proportions as COVID-19 collides with a surge in other infectious diseases. The widespread growth of SARS, coupled with the co-circulation of COVID-19 and Influenza A, underscores the urgent need for comprehensive public health measures, increased testing, and robust healthcare infrastructure.
As the nation grapples with this multifaceted challenge, coordinated efforts at local, regional, and national levels are imperative. The findings from the Fiocruz InfoGripe Bulletin serve as a stark reminder that Brazil's healthcare system is on the brink, necessitating immediate and sustained interventions to prevent further escalation of the crisis.
Brazil’s Healthcare Doomed As COVID-19 Infections Rise Along With Dengue, Flu, RSV, Malaria, Zika, Measles, TB, HIV And Cholera Infections
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 04, 2024
As Brazil grapples with the relentless onslaught of the COVID-19 pandemic, recent data released by the Fiocruz InfoGripe Bulletin paints a grim picture of the country's healthcare system. The report, unveiled on February 29th, reveals a concerning surge in COVID-19 cases, with an alarming twist. Not only is the COVID-19 crisis escalating, but Brazil is also witnessing a simultaneous rise in infections of Dengue, Malaria, Measles, Tuberculosis (TB), Human Immunodeficiency Virus (HIV), and Cholera.
Local COVID-19 News coverages show that most hospitals and emergency rooms across Brazil are inundated with sick individuals and causing a near collapse of the country’s public healthcare infrastructure.
Worrisome Regional Trends
The bulletin identifies a significant increase in respiratory infections and pneumonia cases linked to COVID-19 across the Central-South regions of Brazil. The Southeast, Central-West, and South regions are particularly hard-hit, displaying clear indicators of an upswing in COVID-19-related respiratory distress. Disturbingly, most states in the Center-South exhibit this upward trajectory, hinting at a widespread and escalating health crisis.
The Northeastern states are not immune to the surge, with some displaying signs of increased SARS, albeit the infectious agent responsible remains unclear. In Bahia, however, there is a notable association with influenza A, commonly known as the flu virus. The scenario raises concerns about potential co-circulation of viruses, complicating the healthcare landscape further.
Loading…
agencia.fiocruz.br
Expert Analysis and Recommendations
Marcelo Gomes, a researcher from the Scientific Computing Program and coordinator of InfoGripe, emphasizes the gravity of the situation. Gomes underscores the national concern, emphasizing the troublesome co-circulation of COVID-19 and Influenza A in several Central-South states. Despite COVID-19 causing a significantly higher number of hospitalizations than the flu, the simultaneous circulation of both viruses poses unprecedented challenges to the already strained healthcare infrastructure.
Gomes reiterates the importance of adhering to preventive measures, urging individuals with respiratory infection symptoms to stay at home and rest. For those compelled to venture outside, the use of appropriate masks, such as PFF2 or N95, is strongly advised to curb virus transmission, especially when visiting healthcare facilities.
National Overview of COVID-19
Examining both long-term (last six weeks) and short-term (last three weeks) trends, the report identifies an alarming growth in respiratory infections incidence and mortality associated with COVID-19. Over the last eight weeks, the impact of respiratory infections remains most pronounced among young children and the elderly, with COVID-19 disproportionately affecting those under two years old and individuals over 65.
The report highlights other respiratory viruses, such as Respiratory Syncytial Virus (RSV) and rhinovirus, as significant contributors to respiratory infections incidence in young children. However, the mortality rates for respiratory infections, particularly related to COVID-19, remain significantly higher in the elderly population.
Regional Breakdown of Respiratory Infection Increases
Eighteen states exhibit concerning signs of long-term respiratory infections growth, including Bahia, Ceará, Distrito Federal, Espírito Santo, Goiás, Maranhão, Mato Grosso, Mato Grosso do Sul, Minas Gerais, Pará, Paraíba, Paraná, Rio Grande do Sul, Rio de Janeiro, Roraima, Santa Catarina, Sergipe, and São Paulo.
Specifically related to respiratory infection cases due to COVID-19, the Federal District, Espírito Santo, Goiás, Minas Gerais, Mato Grosso, Mato Grosso do Sul, Paraná, Rio de Janeiro, Rio Grande do Sul, Santa Catarina, and São Paulo display an alarming increase.
In Bahia, Rio de Janeiro, Rio Grande do Sul, Santa Catarina, and São Paulo, there is evidence of increased respiratory infections caused by influenza A (flu). In some states like Ceará, Maranhão, Pará, Paraíba, and Roraima, the rise in respiratory infections is concentrated among children, with the responsible viral agent yet to be determined.
City-Specific Concerns
Seventeen capitals across Brazil are witnessing a surge in severe respiratory infection cases, including Aracaju (SE), Belém (PA), Boa Vista (RR), Campo Grande (MS), Cuiabá (MT), Curitiba (PR), Florianópolis (SC), Fortaleza (CE), Goiânia (GO), João Pessoa (PB), Maceió (AL), Porto Velho (RO), Rio de Janeiro (RJ), Salvador (BA), São Luís (MA), São Paulo (SP), and Vitória (ES).
Respiratory Virus Prevalence and Mortality
Over the past four epidemiological weeks, the prevalence among cases with positive results for respiratory viruses included influenza A (10.3%), influenza B (0.3%), RSV (10.8%), and Sars-CoV-2/Covid-19 (70.6%). Among deaths, these viruses were present in influenza A (2.5%), influenza B (0.6%), RSV (0.6%), and SARS-CoV-2/COVID-19 (92.5%).
In the epidemiological year 2024, 10,985 Respiratory infection cases have been reported, with 37.7% having a positive laboratory result for a respiratory virus. COVID-19 dominates, comprising 69.6% of positive cases. Despite ongoing investigations, the fluid nature of case notifications and laboratory result insertions necessitates ongoing updates.
SARS-CoV-2 Variants At Play In Brazil
Based on data collated by Thailand Medical News, the predominating SARS-CoV-2 sub-lineages circulating in Brazil at the moment are JN.2.5, JN.1.7, JN.1.1 and JN.1.
Dengue Rising at exponential rates in Brazil
Refer:
Loading…
www.thailandmedical.news
Conclusion
Brazil is facing a healthcare crisis of unprecedented proportions as COVID-19 collides with a surge in other infectious diseases. The widespread growth of SARS, coupled with the co-circulation of COVID-19 and Influenza A, underscores the urgent need for comprehensive public health measures, increased testing, and robust healthcare infrastructure.
As the nation grapples with this multifaceted challenge, coordinated efforts at local, regional, and national levels are imperative. The findings from the Fiocruz InfoGripe Bulletin serve as a stark reminder that Brazil's healthcare system is on the brink, necessitating immediate and sustained interventions to prevent further escalation of the crisis.
Heliobas Disciple
TB Fanatic
A page up I was wondering how many shots we were up to. I undercounted..... apparently it's NINE.

 www.dossier.today
(fair use applies)
www.dossier.today
(fair use applies)
Dose number NINE: CDC panel green lights yet another Covid mRNA shot
For the vax compliant, that's nine doses in only three years.
Jordan Schachtel
Feb 29, 2024
For the Americans out there who remain true to the CDC’s vaccine recommendation schedule, you’ll be heading over to your local clinic in the coming weeks for another dose of Pfizer or Moderna’s mRNA Covid gene serum.
On Wednesday, the CDC recommended that seniors get another “booster” in the Spring, making this the ninth dose for Americans who continue to abide by the Government Health booster guidance schedule.
In just three year’s time, the CDC’s vaccine advisory committee has now authorized nine separate injections of a shot that was once advertised as the cure to the coronavirus.
“Today’s recommendation allows older adults to receive an additional dose of this season’s COVID-19 vaccine to provide added protection,” said CDC Director Mandy Cohen. “Most COVID-19 deaths and hospitalizations last year were among people 65 years and older. An additional vaccine dose can provide added protection that may have decreased over time for those at highest risk.”
Government bureaucrats have taken pains to muddy the waters around the fact that this would be the ninth shot for those on schedule, but it is indeed the ninth shot, according to The Dossier’s calculations.
As you can see above, we’re the only publication, as far as we’re aware, that’s been running the numbers this whole time. The FDA and CDC have taken significant measures to deceive the public, by resetting the counter every time Pharma spins up another mRNA shot that they say is better targeted for the new variants.
And the Pharma-sponsored corporate media always does them a solid in helping with the advertising process.

Speaking of new variants.
The ninth shot, which is currently only recommended for seniors, but will soon be authorized for all ages, is considered a booster that targets the Eris variant, or EG.5.
But what Pfizer and Moderna don’t want you to find out is that the Eris variant no longer exists. The data for this comes directly from the CDC.
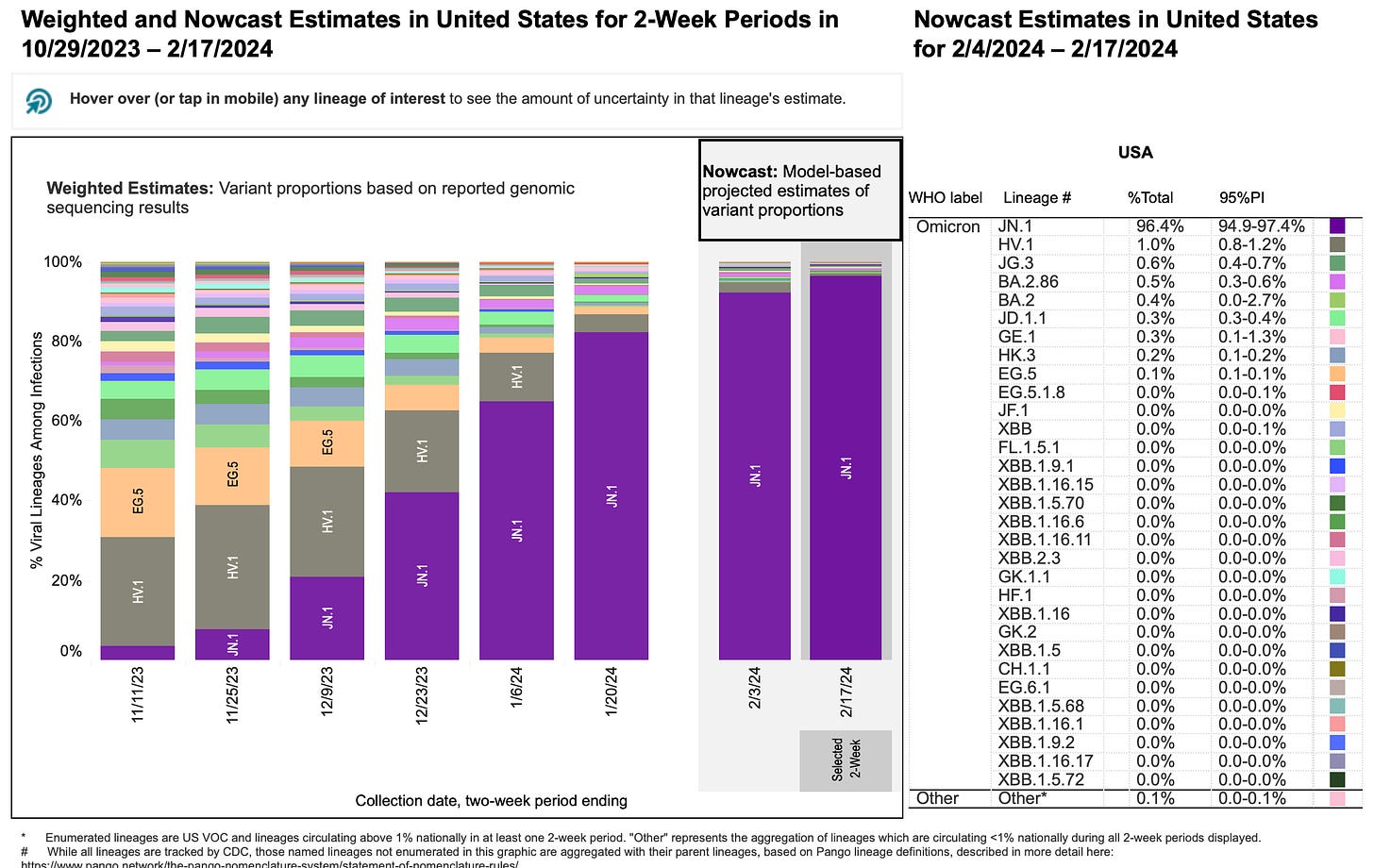
As you can see in the above CDC Variant Tracker, the EG.5 variant is no longer found in the United States.
However, in order to combat the reality of expired vaccines, pharmaceutical companies have conducted shoddy studies that advance the idea that the new shots offer “protection” from the latest variants, despite these variants not being detected when the shots were being formulated.

It’s official: the Pfizer loyalty card has become a reality. Nine shots in three years.
.
This is the news of today. Just reporting. How many boosters are we up to now? For a vaccine that doesn't stop you from getting or transmitting it? I think this makes 6 but I could be miscounting.
(fair use applies)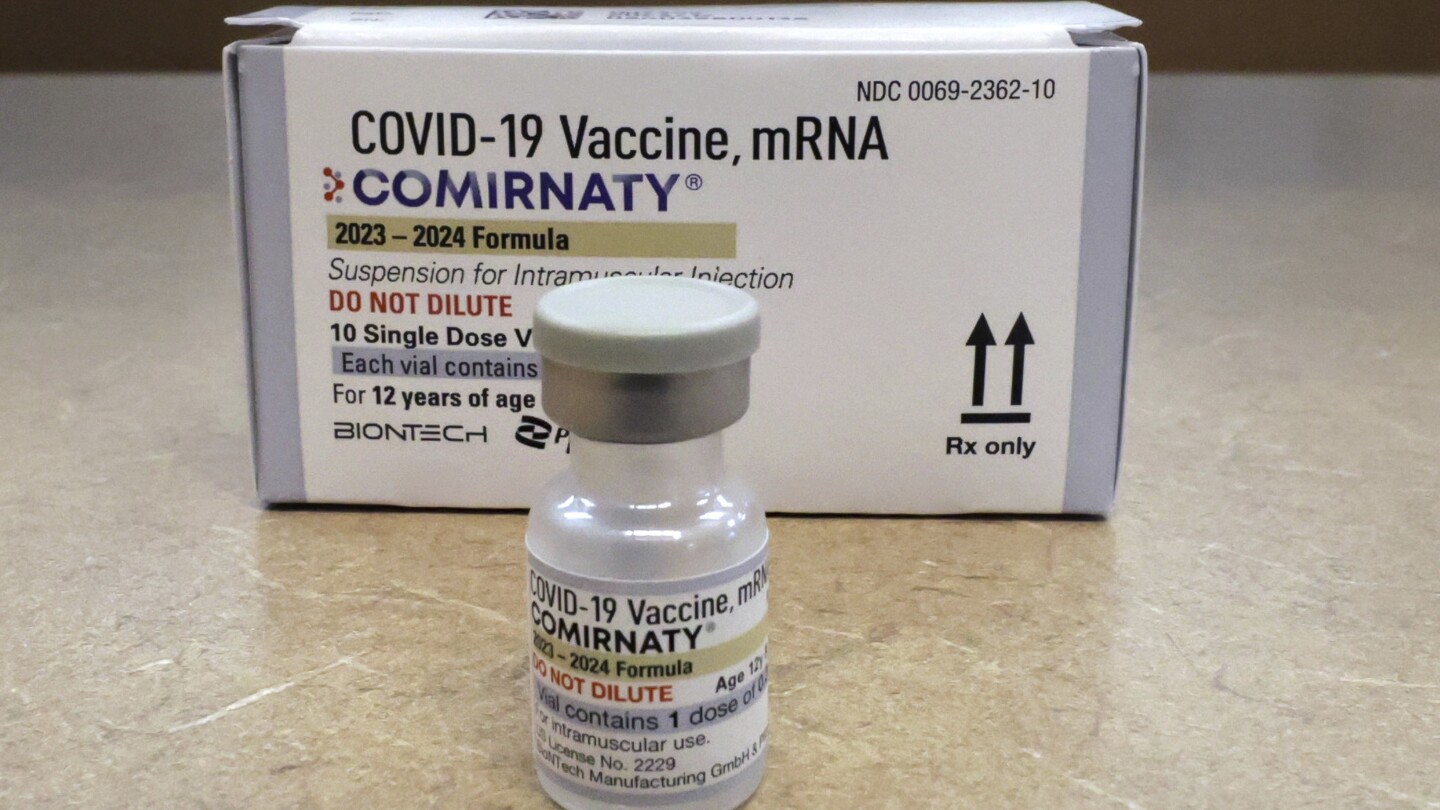
Older US adults should get another COVID-19 shot, health officials recommend
Federal health officials say older U.S. adults who got a COVID-19 shot in the fall should get a booster dose now.apnews.com
Older US adults should get another COVID-19 shot, health officials recommend
By MIKE STOBBE
February 28, 2024
NEW YORK (AP) — Older U.S. adults should roll up their sleeves for another COVID-19 shot, even if they got a booster in the fall, U.S. health officials said Wednesday.
The Centers for Disease Control and Prevention said Americans 65 and older should get another dose of the updated vaccine that became available in September — if at least four months has passed since their last shot. In making the recommendation, the agency endorsed guidance proposed by an expert advisory panel earlier in the day.
“Most COVID-19 deaths and hospitalizations last year were among people 65 years and older. An additional vaccine dose can provide added protection ... for those at highest risk,” CDC Director Dr. Mandy Cohen said in a statement.
The advisory panel’s decision came after a lengthy discussion about whether to say older people “may” get the shots or if they “should” do so. That reflects a debate among experts about how necessary another booster is and whether yet another recommendation would add to the public’s growing vaccine fatigue.
Some doctors say most older adults are adequately protected by the fall shot, which built on immunity derived from earlier vaccinations and exposure to the virus itself. And preliminary studies so far have shown no substantial waning in vaccine effectiveness over six months.
However, the body’s vaccine-induced defenses tend to fade over time, and that happens faster in seniors than in other adults. The committee had recommended COVID-19 booster doses for older adults in 2022 and 2023.
COVID-19 remains a danger, especially to older people and those with underlying medical conditions. There are still more than 20,000 hospitalizations and more than 2,000 deaths each week due to the coronavirus, according to the CDC. And people 65 and older have the highest hospitalization and death rates.
Some members of the advisory panel said a “should” recommendation is meant to more clearly prod doctors and pharmacists to offer the shots.
“Most people are coming in either wanting the vaccine or not,” said Dr. Jamie Loehr, a committee member and family doctor in Ithaca, New York. “I am trying to make it easier for providers to say, ‘Yes, we recommend this.’”
In September, the government recommended a new COVID-19 shot recipe built against a version of the coronavirus called XBB.1.5. That single-target vaccine replaced combination shots that had been targeting both the original coronavirus strain and a much earlier omicron version.
The CDC recommended the new shots for everyone 6 months and older, and allowed that people with weak immune systems could get a second dose as early as two months after the first.
Most Americans haven’t listened. According to the latest CDC data, 13% of U.S. children have gotten the shots and about 22% of U.S. adults have. The vaccination rate is higher for adults 65 and older, at nearly 42%.
“In each successive vaccine, the uptake has gone down,” said Dr. David Canaday, a Case Western Reserve University infectious diseases expert who studies COVID-19 in older people.
“People are tired of getting all these shots all the time,” said Canaday, who does not serve on the committee. “We have to be careful about over-recommending the vaccine.”
But there is a subset of Americans — those at higher danger of severe illness and death — who have been asking if another dose is permissible, said Dr. William Schaffner, a Vanderbilt University vaccines expert who serves on a committee workgroup that has been debating the booster question.
Indeed, CDC survey data suggests that group’s biggest worry about the vaccine is whether it’s effective enough.
Agency officials say that among those who got the latest version of the COVID-19 vaccine, 50% fewer will get sick after they come into contact with the virus compared with those who didn’t get the fall shot.

Dose number NINE: CDC panel green lights yet another Covid mRNA shot
For the vax compliant, that's nine doses in only three years.
Dose number NINE: CDC panel green lights yet another Covid mRNA shot
For the vax compliant, that's nine doses in only three years.
Jordan Schachtel
Feb 29, 2024
For the Americans out there who remain true to the CDC’s vaccine recommendation schedule, you’ll be heading over to your local clinic in the coming weeks for another dose of Pfizer or Moderna’s mRNA Covid gene serum.
On Wednesday, the CDC recommended that seniors get another “booster” in the Spring, making this the ninth dose for Americans who continue to abide by the Government Health booster guidance schedule.
In just three year’s time, the CDC’s vaccine advisory committee has now authorized nine separate injections of a shot that was once advertised as the cure to the coronavirus.
“Today’s recommendation allows older adults to receive an additional dose of this season’s COVID-19 vaccine to provide added protection,” said CDC Director Mandy Cohen. “Most COVID-19 deaths and hospitalizations last year were among people 65 years and older. An additional vaccine dose can provide added protection that may have decreased over time for those at highest risk.”
Government bureaucrats have taken pains to muddy the waters around the fact that this would be the ninth shot for those on schedule, but it is indeed the ninth shot, according to The Dossier’s calculations.
August 17, 2023
April 19, 2023
March 30, 2022
March 29, 2022
As you can see above, we’re the only publication, as far as we’re aware, that’s been running the numbers this whole time. The FDA and CDC have taken significant measures to deceive the public, by resetting the counter every time Pharma spins up another mRNA shot that they say is better targeted for the new variants.
And the Pharma-sponsored corporate media always does them a solid in helping with the advertising process.

Speaking of new variants.
The ninth shot, which is currently only recommended for seniors, but will soon be authorized for all ages, is considered a booster that targets the Eris variant, or EG.5.
But what Pfizer and Moderna don’t want you to find out is that the Eris variant no longer exists. The data for this comes directly from the CDC.
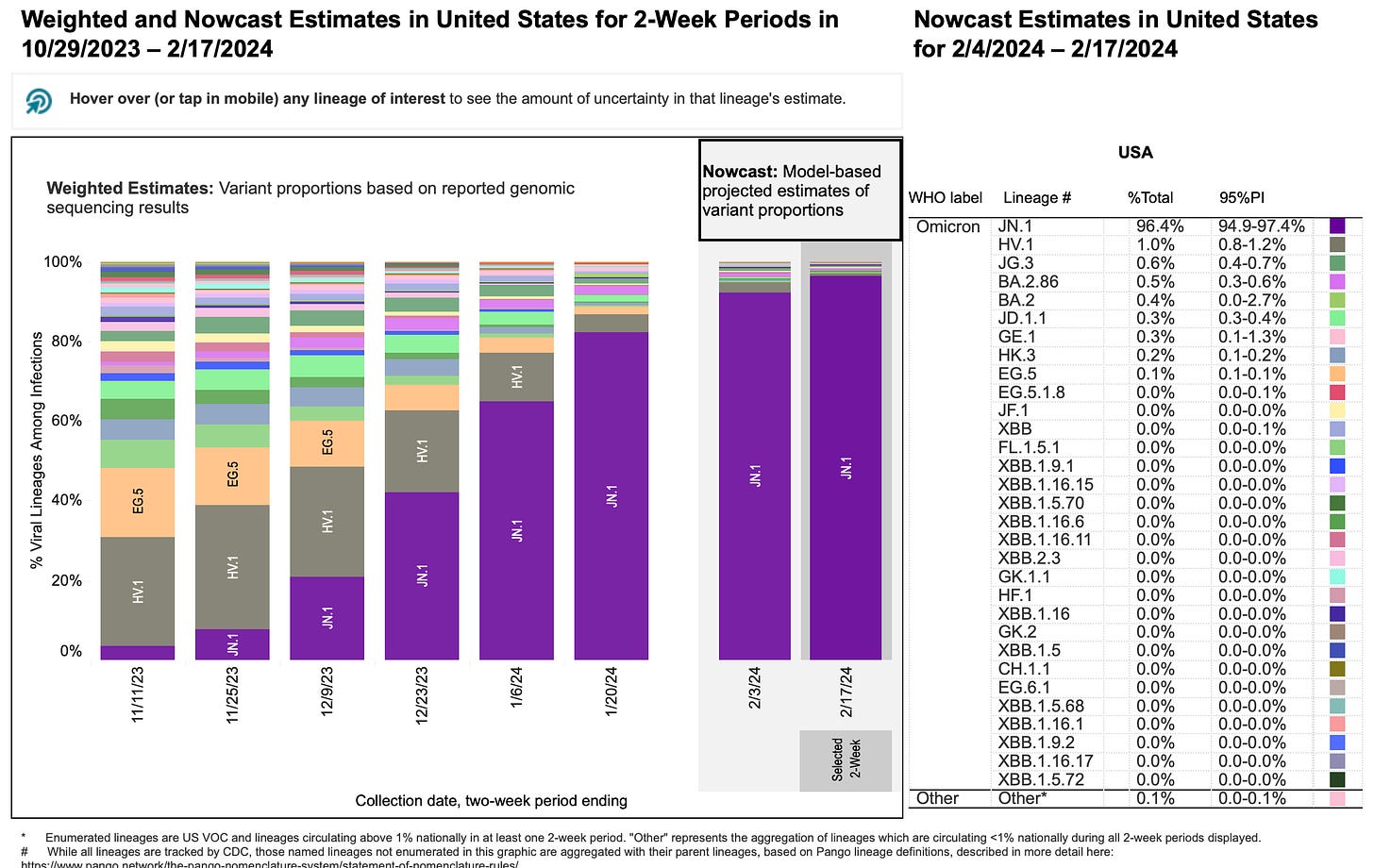
As you can see in the above CDC Variant Tracker, the EG.5 variant is no longer found in the United States.
However, in order to combat the reality of expired vaccines, pharmaceutical companies have conducted shoddy studies that advance the idea that the new shots offer “protection” from the latest variants, despite these variants not being detected when the shots were being formulated.

It’s official: the Pfizer loyalty card has become a reality. Nine shots in three years.
.
Heliobas Disciple
TB Fanatic
There is a new Geert interview with Dr. Philip McMillan. They talk about Geert's new course for about the first 10 minutes, but then he gets into what's happening with JN.1. He says it was a mistake to put a date on his prediction, but he still stands by it. He says immune refocusing gave the immune system a chance to mitigate against more infectiousness. That's why the timeline didn't happen. But the virus continues to evolve. And as its spreading within the host's different organs, it will accumulate to a limit where the evolution will be exponential. He didn't think it would take 3 or 4 months. Now he's cautiously says end of March and he probably shouldn't do that because what's happening is unprecedented. But it's a very dangerous situation, the pressure is mounting. There is no precedent, can't draw parallels and so shouldn't put a date. Philip asked if Geert agrees with the CDC saying go back to normal. Geert says he understands their reaction, that finally they realize that whatever they do they cannot and they did not and they will not control the virus. They maybe managed to delay the whole thing a little bit but Geert says they can't delay it much longer. His answer though is the only thing you can do without herd immunity is massively administering anti-virals to highly vaccinated population, but those have to work and you have to do it on a large scale. But he knows they won't do it. They have no candidate that's eligible for large scale prophylactic administration. So it doesn't make sense to leave the measures in place. They're not testing, they're not doing sequencing, so why keep the measures in place. They finally realize this is complete nonsense and has been so from the very beginning. A follow up video should hopefully happen in about a month.
View: https://www.youtube.com/watch?v=lS4gZSsQnnI
Support Geert - Natural and immune escape pandemics/epidemics
Vejon Health
Streamed live March 3, 2024
30 min 38 sec
The immune biology of natural and immune escape pandemics/epidemics Course - UPDATED!
Register Here:
ANH Health Creation Faculty...
Further Geert information here:
https://www.voiceforscienceandsolidar...
In this second running of this unique deep dive into the immune biology of epidemics and pandemics, Dr Vanden Bossche will bring new insights and updated material in order to provide comprehensive insights into the intricate interplay between pathogens and the host immune system. If you would like a comprehensive understanding how this natural interaction influences the evolutionary dynamics of viral immune evasion and the adaptive responses of the host immune system at a population level, then you can’t afford to miss this course. Even if you were one of the lucky ones to join Dr Vanden Bossche’s first course in 2023, attending again will deepen your knowledge base, give you new insights in this very complex area and allow you to interact once more with Dr Vanden Bossche and have your questions answered.
Support Geert - Natural and immune escape pandemics/epidemics
Vejon Health
Streamed live March 3, 2024
30 min 38 sec
The immune biology of natural and immune escape pandemics/epidemics Course - UPDATED!
Register Here:
ANH Health Creation Faculty...
Further Geert information here:
https://www.voiceforscienceandsolidar...
In this second running of this unique deep dive into the immune biology of epidemics and pandemics, Dr Vanden Bossche will bring new insights and updated material in order to provide comprehensive insights into the intricate interplay between pathogens and the host immune system. If you would like a comprehensive understanding how this natural interaction influences the evolutionary dynamics of viral immune evasion and the adaptive responses of the host immune system at a population level, then you can’t afford to miss this course. Even if you were one of the lucky ones to join Dr Vanden Bossche’s first course in 2023, attending again will deepen your knowledge base, give you new insights in this very complex area and allow you to interact once more with Dr Vanden Bossche and have your questions answered.
Heliobas Disciple
TB Fanatic
White House lifting its COVID-19 testing rule for people around Biden, ending a pandemic vestige
The White House has lifted its COVID-19 testing requirement for those who plan to be in close contact with President Joe Biden, Vice President Kamala Harris and their spouses.
White House lifting its COVID-19 testing rule for people around Biden, ending a pandemic vestige
By ZEKE MILLER
March 4, 2024
WASHINGTON (AP) — The White House on Monday lifted its COVID-19 testing requirement for those who plan to be in close contact with President Joe Biden, Vice President Kamala Harris and their spouses, bringing to an end the last coronavirus prevention protocol at the White House.
The White House said the change aligns its policies with the Centers for Disease Control and Prevention guidance. The agency last week relaxed its recommendation that those who test positive for COVID-19 isolate for five days. Now, the agency says people can return to work or regular activities if their symptoms are mild and improving and it’s been a day since they’ve had a fever.
The White House testing protocol was instituted shortly after the pandemic began in 2020 when former President Donald Trump was in the White House. It was further strengthened by Biden’s administration when he took office amid the pandemic in January 2021.
Both Trump and Biden contracted the virus while in office. Trump required hospitalization after falling seriously ill weeks before the 2020 presidential election; Biden had minimal symptoms after catching it in the summer of 2022 after having been vaccinated.
More than 1.18 million people in the U.S. died from COVID-19, according to CDC data and 6.85 million were hospitalized over the past four years. More than 270 million people have received at least one dose of a COVID-19 vaccine in the U.S. The vaccines have helped dramatically reduce instances of serious disease and death since their widespread availability in early 2021.
Heliobas Disciple
TB Fanatic

Free COVID-19 test program to be suspended for now
The federal government’s free at-home COVID-19 test program will be suspended beginning Friday in response to a drop in respiratory diseases. The Biden administration brought back the free test program last year ahead of the respiratory viral season. By going to COVIDtests.gov, households could...
Free COVID-19 test program to be suspended for now
Joseph Choi
Mon, March 4, 2024, 3:59 PM EST
The federal government’s free at-home COVID-19 test program will be suspended beginning Friday in response to a drop in respiratory diseases.
The Biden administration brought back the free test program last year ahead of the respiratory viral season. By going to COVIDtests.gov, households could order a free pack of four at-home COVID-19 tests. This most recent batch of free tests was the sixth round made available.
A banner on the website now states that “ordering for free COVID-19 tests via this website will be suspended after Friday, March 8, 2024. All orders placed on or before March 8 will be delivered.”
The program may be brought back again in the future as needed.
According to federal data, weekly hospital admissions for COVID-19 and weekly deaths have been declining in the U.S. since the start of January.
The most recent weekly flu report from the Centers for Disease Control and Prevention (CDC) indicated a 14.2 percent drop in positive lab tests for influenza in the past week, though it also indicated that “seasonal influenza activity remains elevated nationally,” with increases in activity in some parts of the country.
This announcement shortly after the CDC shifted its coronavirus guidance last week, no longer recommending that people stay home for five days after testing positive for the virus.
The updated guidance now aligns with what health experts recommend for flu or RSV infections, advising people stay home if they are sick and symptomatic, return to normal activities if their symptoms are improving and they are fever-free for 24 hours without medication.
Heliobas Disciple
TB Fanatic
Repeating again. I post articles that are news, not because I agree with them. I am posting this because it's what the 'science' is saying. Just memoralizing it on the thread.

 medicalxpress.com
(fair use applies)
medicalxpress.com
(fair use applies)
Breastfeeding after COVID-19 booster can give babies antibodies, research finds
by Meredith Bauer, University of Florida
March 4, 2024
Lactating mothers who get the COVID-19 booster pass along the antibodies to their children via their breast milk—and potentially protect babies too young to receive the vaccine, a study from the University of Florida Institute of Food and Agricultural Sciences (UF/IFAS) and the UF College of Medicine has found.
The study is the third in a series that looks at antibody protection being transferred via breast milk from mothers who received their first two COVID-19 vaccinations, and now the booster shot. The second publication reported the same antibody transfer via breast milk.
"We think that breast milk may play an important role in protecting the infants during the first six months of life from COVID," said Dr. Vivian Valcarce, a former UF College of Medicine researcher who worked on this study. She now is an assistant professor at the University of Alabama at Birmingham. "We continue to see babies being hospitalized from COVID-19 infections."
The study is published in Frontiers in Nutrition.
The study looked at how breast milk antibody protection changed when a mother received their first COVID-19 booster shot, said Joseph Larkin, UF/IFAS associate professor of microbiology and cell science and part of UF's Emerging Pathogens Institute. Researchers looked at the antibody response and antibody functionality in breast milk and tested to see if antibodies were present after the babies drank breast milk with COVID-19 antibodies.
Larkin said this study suggests that breastfeeding can provide COVID-19 antibodies for infants too young to receive a vaccination—and that the antibodies wane in people's bodies over time, so getting a booster can provide prolonged protection to babies that drink breast milk.
"When babies are born, they have an immature immune system, so they rely heavily on mom's immune system," he said. "Breastfeeding can serve as a gap in between while babies are building their own immune system."
Larkin said some antibodies are transferred to fetuses through the placenta, as well, but that initial protection also lessens over time.
In this study, 14 lactating mothers and their babies were followed from before they received their COVID-19 booster until after they received their booster shots, Larkin said. Researchers tested the mothers' blood to confirm their bodies made COVID-19 antibodies after a booster shot, tested breast milk to confirm the milk had antibodies in it and tested babies' stools to confirm antibodies were present in the babies' bodies.
To see if the breast milk's antibodies worked against COVID-19, breast milk was placed in a 96-well plate with a lab-safe COVID virus strain, and researchers found these antibodies from the mother disable the virus, said Lauren Stafford, a UF/IFAS graduate research assistant and Ph.D. candidate in microbiology and cell science.
The study was a collaboration between UF/IFAS and the UF College of Medicine and included Dr. Josef Neu, professor of pediatrics within the division of neonatology at the UF College of Medicine.
"This shows how important breast milk and breastfeeding is for infant health during a pandemic," Valcarce said.
More information: Vivian Valcarce et al, COVID-19 booster enhances IgG mediated viral neutralization by human milk in vitro, Frontiers in Nutrition (2024). DOI: 10.3389/fnut.2024.1289413
Provided by University of Florida

Breastfeeding after COVID-19 booster can give babies antibodies, research finds
Lactating mothers who get the COVID-19 booster pass along the antibodies to their children via their breast milk—and potentially protect babies too young to receive the vaccine, a study from the University of Florida Institute of Food and Agricultural Sciences (UF/IFAS) and the UF College of...
Breastfeeding after COVID-19 booster can give babies antibodies, research finds
by Meredith Bauer, University of Florida
March 4, 2024
Lactating mothers who get the COVID-19 booster pass along the antibodies to their children via their breast milk—and potentially protect babies too young to receive the vaccine, a study from the University of Florida Institute of Food and Agricultural Sciences (UF/IFAS) and the UF College of Medicine has found.
The study is the third in a series that looks at antibody protection being transferred via breast milk from mothers who received their first two COVID-19 vaccinations, and now the booster shot. The second publication reported the same antibody transfer via breast milk.
"We think that breast milk may play an important role in protecting the infants during the first six months of life from COVID," said Dr. Vivian Valcarce, a former UF College of Medicine researcher who worked on this study. She now is an assistant professor at the University of Alabama at Birmingham. "We continue to see babies being hospitalized from COVID-19 infections."
The study is published in Frontiers in Nutrition.
The study looked at how breast milk antibody protection changed when a mother received their first COVID-19 booster shot, said Joseph Larkin, UF/IFAS associate professor of microbiology and cell science and part of UF's Emerging Pathogens Institute. Researchers looked at the antibody response and antibody functionality in breast milk and tested to see if antibodies were present after the babies drank breast milk with COVID-19 antibodies.
Larkin said this study suggests that breastfeeding can provide COVID-19 antibodies for infants too young to receive a vaccination—and that the antibodies wane in people's bodies over time, so getting a booster can provide prolonged protection to babies that drink breast milk.
"When babies are born, they have an immature immune system, so they rely heavily on mom's immune system," he said. "Breastfeeding can serve as a gap in between while babies are building their own immune system."
Larkin said some antibodies are transferred to fetuses through the placenta, as well, but that initial protection also lessens over time.
In this study, 14 lactating mothers and their babies were followed from before they received their COVID-19 booster until after they received their booster shots, Larkin said. Researchers tested the mothers' blood to confirm their bodies made COVID-19 antibodies after a booster shot, tested breast milk to confirm the milk had antibodies in it and tested babies' stools to confirm antibodies were present in the babies' bodies.
To see if the breast milk's antibodies worked against COVID-19, breast milk was placed in a 96-well plate with a lab-safe COVID virus strain, and researchers found these antibodies from the mother disable the virus, said Lauren Stafford, a UF/IFAS graduate research assistant and Ph.D. candidate in microbiology and cell science.
The study was a collaboration between UF/IFAS and the UF College of Medicine and included Dr. Josef Neu, professor of pediatrics within the division of neonatology at the UF College of Medicine.
"This shows how important breast milk and breastfeeding is for infant health during a pandemic," Valcarce said.
More information: Vivian Valcarce et al, COVID-19 booster enhances IgG mediated viral neutralization by human milk in vitro, Frontiers in Nutrition (2024). DOI: 10.3389/fnut.2024.1289413
Provided by University of Florida
Heliobas Disciple
TB Fanatic
(fair use applies)
MRI Study Reveals High Incidence Of Cerebrovascular Lesions In Children Infected With Omicron Variants
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 05, 2024
The ongoing battle against the COVID-19 pandemic has taken a new turn with the emergence of the Omicron variant. Beyond the well-documented respiratory implications, the virus's impact on neurological health, particularly in pediatric patients, has become increasingly apparent. Recent research covered in this COVID-19 News report, conducted by the National Taiwan University Hospital sheds light on the alarming incidence of cerebrovascular lesions in children infected with the Omicron variant. This retrospective case series, undertaken from April to June 2022, sought to unravel the intricate details of magnetic resonance imaging (MRI) changes in pediatric COVID-19 cases, with a special focus on cerebral vasculature alterations.
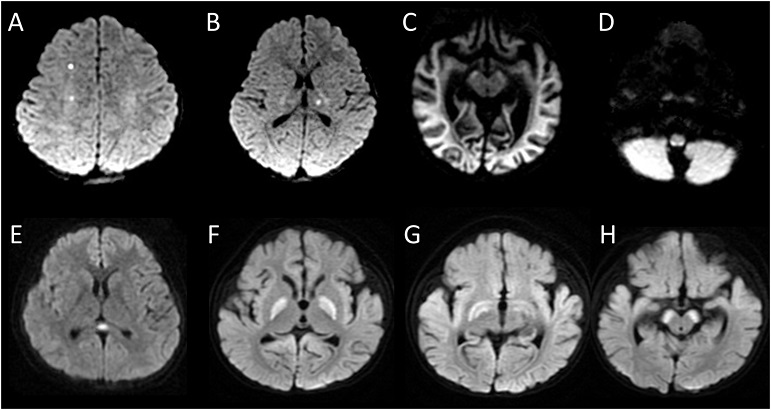
High Incidence Of Cerebrovascular Lesions In Children Infected With Omicron Variants
(A-B) Diffusion-weighted imaging (DWI) of an 8-year-old boy with seizure and encephalopathy showed restricted diffusion at right frontal and left thalamus. (C) DWI of an 8-month-old girl with status epilepticus showed diffuse restricted diffusion over the cerebral cortex and white matter. (D) DWI of a 1-year-old boy with encephalopathy and seizure showed restricted diffusion at the posterior medulla (E) DWI of a 13-year-old boy with ataxia, nystagmus and encephalopathy showed restricted diffusion at the splenium of the corpus callosum. (F-H) DWI of an 11-month-old girl with seizure and coma showed restricted diffusion at bilateral globus pallidus, subthalamic regions, and cerebral peduncles.
Understanding the Background
Previous studies have highlighted the neurological involvement associated with COVID-19, both in adults and children. The Omicron variant, known for its heightened transmissibility, has brought forth a surge in pediatric hospitalizations, prompting an urgent need for a deeper understanding of the neurological impact in this demographic. While earlier variants of the virus were linked to various neurological abnormalities, the specific MRI changes and cerebrovascular implications of the Omicron variant in pediatric patients remained largely unexplored until now.
Methodology and Findings
The study, involving 31 pediatric patients with neurological symptoms during Omicron infection, revealed MRI abnormalities in nearly half of the cases (48.4%). The predominant abnormality was identified as encephalitis/encephalopathy in 73.3% of cases. Noteworthy MRI findings included focal diffusion-weighted imaging (DWI) hyperintensity in the cerebral cortex and thalamus, diffuse cortical T2/DWI hyperintensity, and lesions in various brain regions such as the medulla, pons, cerebellum, and splenium of corpus callosum.
Vascular abnormalities were a striking feature in 80% of patients with MRI abnormalities, primarily affecting the middle cerebral arteries. The spectrum of neurological manifestations ranged from seizures to the intriguin g Alice in Wonderland syndrome, emphasizing the diverse impact of COVID-19 on pediatric patients.
Demographics and Clinical Characteristics
The demographic breakdown of the study cohort comprised 11 females and 20 males, with a median age of 6 years (ranging from 3 months to 13 years). All patients presented with fever and/or upper respiratory symptoms, without acute respiratory distress syndrome or severe non-neurological manifestations. Neurological symptoms included seizures, visual hallucinations, altered mental status, headache, myoclonus, hemiplegia, tics, gait disturbance, and parasomnia.
MRI Abnormalities and Vascular Involvement
Among the 31 patients, 15 exhibited MRI abnormalities, with diagnoses spanning encephalitis/encephalopathy, ischemic stroke, hemorrhage, and Alice in Wonderland syndrome. Vascular abnormalities were particularly prominent, affecting 80% of patients with MRI abnormalities and primarily involving the anterior cerebral arteries, middle cerebral arteries, posterior cerebral arteries, and internal carotid arteries.
Neurological Outcomes
A subset of patients (4 out of 15) experienced poor neurological outcomes, with a Pediatric Cerebral Performance Category (PCPC) scale of =3 at the last follow-up. Notably, all patients with poor outcomes had abnormal MRIs, emphasizing the potential link between MRI abnormalities and adverse neurological prognosis.
Discussion: Unveiling the Mechanisms
The study's findings shed light on the distinctive MRI abnormalities seen in pediatric patients during the Omicron variant outbreak. These abnormalities paralleled those observed in earlier COVID-19 variants, including inflammatory changes, cytotoxic lesions, hemorrhages, and infarctions. However, the study identified a high prevalence of abnormal MR angiography in medium or large intracerebral vessels (80%) and infarctions in small vessels (8.8%).
The proposed mechanisms for vascular involvement included systemic post-infectious vasculitis, similar to that seen in Multisystemic Inflammatory Syndrome in Children (MIS-C). Cerebral vasculitis affecting small and medium-sized vessels emerged as a significant contributor to brain damage in children infected with the Omicron variant.
Seizures, a prominent neurological manifestation in these cases, were closely associated with abnormal MR angiography, suggesting that vasculitis or vasculopathy might be a crucial mechanism behind the heightened incidence of seizures in Omicron-infected children.
Implications and Future Considerations
The study's comprehensive examination of pediatric COVID-19 cases during the Omicron variant outbreak underscores the need for heightened awareness of neurological manifestations. The observed cerebrovascular abnormalities highlight the complex interplay between the virus and the vascular system in pediatric patients, even in the absence of severe pulmonary disease.
While the study offers valuable insights, the limited focus on patients with relatively severe neurological manifestations calls for further research to explore the prevalence of vascular involvement in children with milder neurological symptoms. Additionally, ongoing monitoring and research are crucial to understand the evolving landscape of COVID-19 and its impact on various patient populations.
Conclusion
In conclusion, the high incidence of cerebrovascular lesions revealed by this MRI study emphasizes the intricate neurological consequences of Omicron variant infection in pediatric patients. Vasculopathy emerges as a pivotal mechanism, contributing to diverse neurological manifestations, including seizures. These findings underscore the importance of vigilance in recognizing and managing neurological complications in pediatric COVID-19 cases. As the global community continues to grapple with the evolving landscape of the pandemic, ongoing research remains paramount in unraveling the complexities of the virus's impact on diverse patient populations, ensuring informed and effective healthcare strategies.
The study findings were published in the peer reviewed Journal of the Formosan Medical Association.
MRI Study Reveals High Incidence Of Cerebrovascular Lesions In Children Infected With Omicron Variants
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 05, 2024
The ongoing battle against the COVID-19 pandemic has taken a new turn with the emergence of the Omicron variant. Beyond the well-documented respiratory implications, the virus's impact on neurological health, particularly in pediatric patients, has become increasingly apparent. Recent research covered in this COVID-19 News report, conducted by the National Taiwan University Hospital sheds light on the alarming incidence of cerebrovascular lesions in children infected with the Omicron variant. This retrospective case series, undertaken from April to June 2022, sought to unravel the intricate details of magnetic resonance imaging (MRI) changes in pediatric COVID-19 cases, with a special focus on cerebral vasculature alterations.
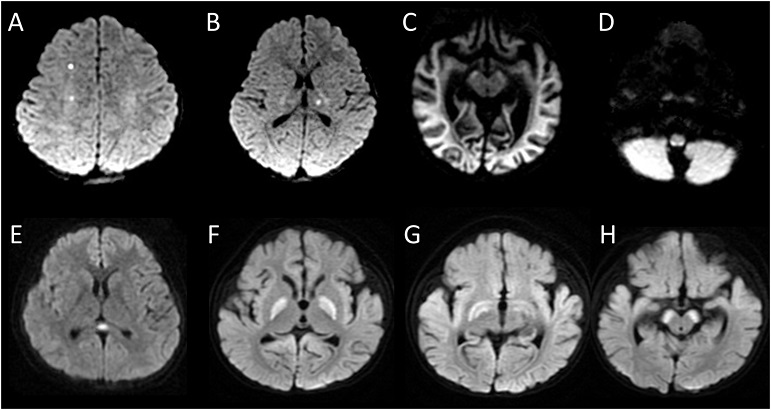
High Incidence Of Cerebrovascular Lesions In Children Infected With Omicron Variants
(A-B) Diffusion-weighted imaging (DWI) of an 8-year-old boy with seizure and encephalopathy showed restricted diffusion at right frontal and left thalamus. (C) DWI of an 8-month-old girl with status epilepticus showed diffuse restricted diffusion over the cerebral cortex and white matter. (D) DWI of a 1-year-old boy with encephalopathy and seizure showed restricted diffusion at the posterior medulla (E) DWI of a 13-year-old boy with ataxia, nystagmus and encephalopathy showed restricted diffusion at the splenium of the corpus callosum. (F-H) DWI of an 11-month-old girl with seizure and coma showed restricted diffusion at bilateral globus pallidus, subthalamic regions, and cerebral peduncles.
Understanding the Background
Previous studies have highlighted the neurological involvement associated with COVID-19, both in adults and children. The Omicron variant, known for its heightened transmissibility, has brought forth a surge in pediatric hospitalizations, prompting an urgent need for a deeper understanding of the neurological impact in this demographic. While earlier variants of the virus were linked to various neurological abnormalities, the specific MRI changes and cerebrovascular implications of the Omicron variant in pediatric patients remained largely unexplored until now.
Methodology and Findings
The study, involving 31 pediatric patients with neurological symptoms during Omicron infection, revealed MRI abnormalities in nearly half of the cases (48.4%). The predominant abnormality was identified as encephalitis/encephalopathy in 73.3% of cases. Noteworthy MRI findings included focal diffusion-weighted imaging (DWI) hyperintensity in the cerebral cortex and thalamus, diffuse cortical T2/DWI hyperintensity, and lesions in various brain regions such as the medulla, pons, cerebellum, and splenium of corpus callosum.
Vascular abnormalities were a striking feature in 80% of patients with MRI abnormalities, primarily affecting the middle cerebral arteries. The spectrum of neurological manifestations ranged from seizures to the intriguin g Alice in Wonderland syndrome, emphasizing the diverse impact of COVID-19 on pediatric patients.
Demographics and Clinical Characteristics
The demographic breakdown of the study cohort comprised 11 females and 20 males, with a median age of 6 years (ranging from 3 months to 13 years). All patients presented with fever and/or upper respiratory symptoms, without acute respiratory distress syndrome or severe non-neurological manifestations. Neurological symptoms included seizures, visual hallucinations, altered mental status, headache, myoclonus, hemiplegia, tics, gait disturbance, and parasomnia.
MRI Abnormalities and Vascular Involvement
Among the 31 patients, 15 exhibited MRI abnormalities, with diagnoses spanning encephalitis/encephalopathy, ischemic stroke, hemorrhage, and Alice in Wonderland syndrome. Vascular abnormalities were particularly prominent, affecting 80% of patients with MRI abnormalities and primarily involving the anterior cerebral arteries, middle cerebral arteries, posterior cerebral arteries, and internal carotid arteries.
Neurological Outcomes
A subset of patients (4 out of 15) experienced poor neurological outcomes, with a Pediatric Cerebral Performance Category (PCPC) scale of =3 at the last follow-up. Notably, all patients with poor outcomes had abnormal MRIs, emphasizing the potential link between MRI abnormalities and adverse neurological prognosis.
Discussion: Unveiling the Mechanisms
The study's findings shed light on the distinctive MRI abnormalities seen in pediatric patients during the Omicron variant outbreak. These abnormalities paralleled those observed in earlier COVID-19 variants, including inflammatory changes, cytotoxic lesions, hemorrhages, and infarctions. However, the study identified a high prevalence of abnormal MR angiography in medium or large intracerebral vessels (80%) and infarctions in small vessels (8.8%).
The proposed mechanisms for vascular involvement included systemic post-infectious vasculitis, similar to that seen in Multisystemic Inflammatory Syndrome in Children (MIS-C). Cerebral vasculitis affecting small and medium-sized vessels emerged as a significant contributor to brain damage in children infected with the Omicron variant.
Seizures, a prominent neurological manifestation in these cases, were closely associated with abnormal MR angiography, suggesting that vasculitis or vasculopathy might be a crucial mechanism behind the heightened incidence of seizures in Omicron-infected children.
Implications and Future Considerations
The study's comprehensive examination of pediatric COVID-19 cases during the Omicron variant outbreak underscores the need for heightened awareness of neurological manifestations. The observed cerebrovascular abnormalities highlight the complex interplay between the virus and the vascular system in pediatric patients, even in the absence of severe pulmonary disease.
While the study offers valuable insights, the limited focus on patients with relatively severe neurological manifestations calls for further research to explore the prevalence of vascular involvement in children with milder neurological symptoms. Additionally, ongoing monitoring and research are crucial to understand the evolving landscape of COVID-19 and its impact on various patient populations.
Conclusion
In conclusion, the high incidence of cerebrovascular lesions revealed by this MRI study emphasizes the intricate neurological consequences of Omicron variant infection in pediatric patients. Vasculopathy emerges as a pivotal mechanism, contributing to diverse neurological manifestations, including seizures. These findings underscore the importance of vigilance in recognizing and managing neurological complications in pediatric COVID-19 cases. As the global community continues to grapple with the evolving landscape of the pandemic, ongoing research remains paramount in unraveling the complexities of the virus's impact on diverse patient populations, ensuring informed and effective healthcare strategies.
The study findings were published in the peer reviewed Journal of the Formosan Medical Association.
Heliobas Disciple
TB Fanatic
(fair use applies)
Thailand Medical Researchers Find That Up To 22.67 Percent Of Cats Tested During The Last Five COVID-19 Waves Were Seropositive
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 05, 2024
In the wake of the unprecedented COVID-19 pandemic, understanding the dynamics of SARS-CoV-2 transmission has become a crucial aspect of public health research. Beyond human-to-human transmission, emerging evidence has pointed towards the potential transmission of the virus from humans to animals, specifically, our feline companions. Thailand, experiencing five waves of COVID-19 outbreaks from December 2020 to March 2022, became a unique setting for a study conducted by researchers from Kasetsart University-Thailand, Thammasat University-Thailand, Colorado State University-USA and the University of Bari-Italy.. The study covered in this Thailand Medical
news report, aimed to delve into the intricate interplay between human and feline populations, shedding light on the transmission dynamics of SARS-CoV-2 in cats.
Objectives and Background
The primary objectives of the research were ambitious, seeking to investigate the prevalence of SARS-CoV-2 antibodies in Thai cats during different epidemic waves, evaluate the effectiveness of a modified human commercial test kit for screening SARS-CoV-2 antibodies in cats, and explore the correlation between cat infections and human epidemic episodes. The backdrop for this study was marked by the atypical case of a veterinarian contracting the virus through close contact with an infected cat, bringing attention to the potential zoonotic transmission pathways.
Empirical evidence from previous studies had suggested an increased susceptibility of cats to SARS-CoV-2. Laboratory experiments had further confirmed their ability to not only contract but also transmit the virus. As a result, the study emphasized the critical need for continuous surveillance to comprehend the dynamics of SARS-CoV-2 transmission in both human and feline populations.
Methods
A meticulous approach was undertaken in collecting and analyzing data for the study. A total of 1107 cat serum samples from various provinces were collected and screened using a modified indirect ELISA human SARS-CoV-2 antibody detection kit. This sophisticated method allowed researchers to examine the presence of antibodies specific to SARS-CoV-2 in feline serum, providing valuable insights into the prevalence of the virus in cat populations. The results were striking, revealing a seropositivity rate of 22.67%, mirroring the trends observed in humans during the five epidemic waves.
To further validate the findings, a cPass™ neutralization test was employed. This test, known for its reliability in confirming the presence of SARS-CoV-2 antibodies, revealed a 3.99% seropositivity rate. The combination of these two tests provided a comprehensive understanding of the prevalence of the virus in cats, allowing researchers to draw correlations with human epidemic episodes.
Results and Correlations
The study revealed distinct patterns among epidemic waves, with Samut Sakhon province in Thailand emerging as a focal point of interest. This province demonstrated a robust positive correlation between the proportion of positive cat sera and human prevalence. Such regional variations underscored the complexity of the interplay between human and feline populations, emphasizing the need for localized investigations to capture the nuances of transmission dynamics.
The correlation between the number of positive cat serum samples and the prevalence of reported human cases was particularly significant in Chon Buri province. Simple linear regression models were employed to test if the prevalence of reported human cases could predict the number of ELISA-positive cat serum samples, revealing a statistically significant relationship. This finding highlighted the potential of using cat populations as indicators for human infections, especially in regions where such correlations were strong.
Discussion
The study's discussion delved into the significance of continuous surveillance for SARS-CoV-2 in both human and feline populations. The potential role of cats as sentinels for human infections was explored, balancing the understanding that owning a domestic cat appears to pose a low risk for additional human infections. The importance of separating cats from infected individuals was emphasized as a preventive measure, despite the seemingly low risk.
The intriguing observation of a decline in cat cases after the fourth wave, amid rising human cases, raised questions about a potential association with the emergence of the Omicron variant. This temporal alignment suggested viral evolution favoring increased human adaptability while potentially reducing feline susceptibility. The discussion acknowledged the need for molecular and epidemiological investigations to shed light on the intricate interplay between viral evolution and host susceptibility.
Conclusion
In conclusion, the comprehensive study on SARS-CoV-2 dynamics in human and feline populations during five outbreak waves in Thailand provided valuable insights into the complex transmission dynamics. Despite certain limitations and challenges in establishing statistical significance, the research emphasized the importance of employing multiple testing methods for accurate assessments during outbreaks. The study underscored the intricate interplay between viral evolution and host susceptibility, offering valuable insights into the localized factors influencing transmission dynamics between humans and cats across different regions.
The findings contribute significantly to our understanding of the complex dynamics of SARS-CoV-2 transmission in both human and feline populations. The potential role of cats as sentinels for human infections, particularly in regions with strong correlations, highlights the need for ongoing surveillance efforts. As the world grapples with the evolving landscape of the COVID-19 pandemic, studies like these pave the way for informed public health strategies and preventive measures. The continuous exploration of the relationship between human and feline infections remains crucial for a comprehensive and effective response to the ongoing challenges posed by the SARS-CoV-2 virus.
The study findings were published in the peer reviewed journal: Animals.

 www.mdpi.com
www.mdpi.com
Thailand Medical Researchers Find That Up To 22.67 Percent Of Cats Tested During The Last Five COVID-19 Waves Were Seropositive
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 05, 2024
In the wake of the unprecedented COVID-19 pandemic, understanding the dynamics of SARS-CoV-2 transmission has become a crucial aspect of public health research. Beyond human-to-human transmission, emerging evidence has pointed towards the potential transmission of the virus from humans to animals, specifically, our feline companions. Thailand, experiencing five waves of COVID-19 outbreaks from December 2020 to March 2022, became a unique setting for a study conducted by researchers from Kasetsart University-Thailand, Thammasat University-Thailand, Colorado State University-USA and the University of Bari-Italy.. The study covered in this Thailand Medical
news report, aimed to delve into the intricate interplay between human and feline populations, shedding light on the transmission dynamics of SARS-CoV-2 in cats.
Objectives and Background
The primary objectives of the research were ambitious, seeking to investigate the prevalence of SARS-CoV-2 antibodies in Thai cats during different epidemic waves, evaluate the effectiveness of a modified human commercial test kit for screening SARS-CoV-2 antibodies in cats, and explore the correlation between cat infections and human epidemic episodes. The backdrop for this study was marked by the atypical case of a veterinarian contracting the virus through close contact with an infected cat, bringing attention to the potential zoonotic transmission pathways.
Empirical evidence from previous studies had suggested an increased susceptibility of cats to SARS-CoV-2. Laboratory experiments had further confirmed their ability to not only contract but also transmit the virus. As a result, the study emphasized the critical need for continuous surveillance to comprehend the dynamics of SARS-CoV-2 transmission in both human and feline populations.
Methods
A meticulous approach was undertaken in collecting and analyzing data for the study. A total of 1107 cat serum samples from various provinces were collected and screened using a modified indirect ELISA human SARS-CoV-2 antibody detection kit. This sophisticated method allowed researchers to examine the presence of antibodies specific to SARS-CoV-2 in feline serum, providing valuable insights into the prevalence of the virus in cat populations. The results were striking, revealing a seropositivity rate of 22.67%, mirroring the trends observed in humans during the five epidemic waves.
To further validate the findings, a cPass™ neutralization test was employed. This test, known for its reliability in confirming the presence of SARS-CoV-2 antibodies, revealed a 3.99% seropositivity rate. The combination of these two tests provided a comprehensive understanding of the prevalence of the virus in cats, allowing researchers to draw correlations with human epidemic episodes.
Results and Correlations
The study revealed distinct patterns among epidemic waves, with Samut Sakhon province in Thailand emerging as a focal point of interest. This province demonstrated a robust positive correlation between the proportion of positive cat sera and human prevalence. Such regional variations underscored the complexity of the interplay between human and feline populations, emphasizing the need for localized investigations to capture the nuances of transmission dynamics.
The correlation between the number of positive cat serum samples and the prevalence of reported human cases was particularly significant in Chon Buri province. Simple linear regression models were employed to test if the prevalence of reported human cases could predict the number of ELISA-positive cat serum samples, revealing a statistically significant relationship. This finding highlighted the potential of using cat populations as indicators for human infections, especially in regions where such correlations were strong.
Discussion
The study's discussion delved into the significance of continuous surveillance for SARS-CoV-2 in both human and feline populations. The potential role of cats as sentinels for human infections was explored, balancing the understanding that owning a domestic cat appears to pose a low risk for additional human infections. The importance of separating cats from infected individuals was emphasized as a preventive measure, despite the seemingly low risk.
The intriguing observation of a decline in cat cases after the fourth wave, amid rising human cases, raised questions about a potential association with the emergence of the Omicron variant. This temporal alignment suggested viral evolution favoring increased human adaptability while potentially reducing feline susceptibility. The discussion acknowledged the need for molecular and epidemiological investigations to shed light on the intricate interplay between viral evolution and host susceptibility.
Conclusion
In conclusion, the comprehensive study on SARS-CoV-2 dynamics in human and feline populations during five outbreak waves in Thailand provided valuable insights into the complex transmission dynamics. Despite certain limitations and challenges in establishing statistical significance, the research emphasized the importance of employing multiple testing methods for accurate assessments during outbreaks. The study underscored the intricate interplay between viral evolution and host susceptibility, offering valuable insights into the localized factors influencing transmission dynamics between humans and cats across different regions.
The findings contribute significantly to our understanding of the complex dynamics of SARS-CoV-2 transmission in both human and feline populations. The potential role of cats as sentinels for human infections, particularly in regions with strong correlations, highlights the need for ongoing surveillance efforts. As the world grapples with the evolving landscape of the COVID-19 pandemic, studies like these pave the way for informed public health strategies and preventive measures. The continuous exploration of the relationship between human and feline infections remains crucial for a comprehensive and effective response to the ongoing challenges posed by the SARS-CoV-2 virus.
The study findings were published in the peer reviewed journal: Animals.

Seroprevalence of Anti-SARS-CoV-2 Antibodies in Cats during Five Waves of COVID-19 Epidemic in Thailand and Correlation with Human Outbreaks
Human-to-animal SARS-CoV-2 transmission was observed, including a veterinarian contracting COVID-19 through close contact with an infected cat, suggesting an atypical zoonotic transmission. This study investigated the prevalence of SARS-CoV-2 antibodies in cats during human outbreaks and...
Heliobas Disciple
TB Fanatic
(fair use applies)
Influence Of Cross-Reactive T Cells In SARS-CoV-2 Infections
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 05, 2024
In the ongoing fight against the COVID-19 pandemic, understanding the intricacies of the immune response has become paramount. One fascinating aspect under intense scrutiny is the role of T cell cross-reactivity – a phenomenon where pre-existing memory T cells, generated in response to diverse infections or vaccinations, exhibit the ability to recognize and mount a response against SARS-CoV-2. This COVID-19 News report delves into the intricate world of T cell cross-reactivity, shedding light on its mechanisms, impact on COVID-19 outcomes, and potential for cross-protection based on a study by researchers from School of Clinical Sciences, Monash University-Australia.
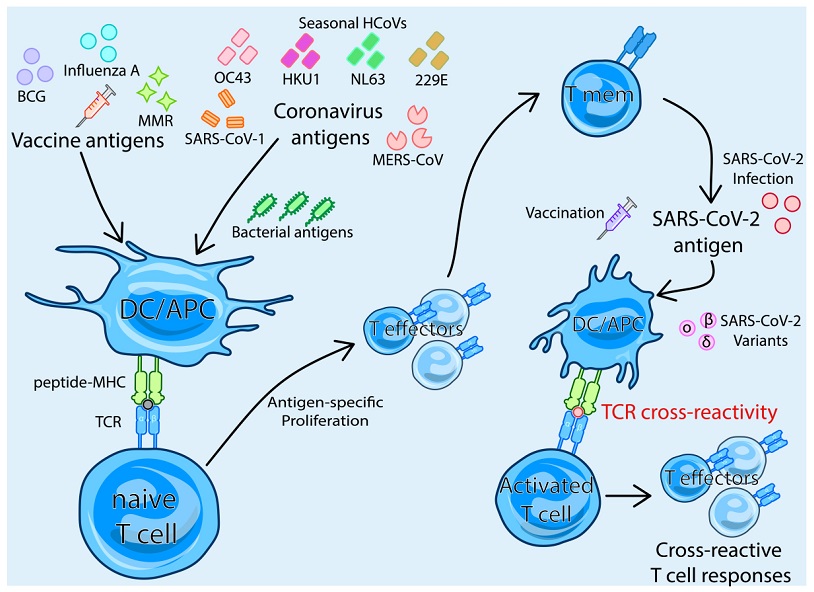
Mechanism of TCR-dependent T cell cross-reactivity with SARS-CoV-2
Adaptive Immune Response to SARS-CoV-2
The Betacoronavirus SARS-CoV-2, responsible for COVID-19, triggers a sophisticated immune response in infected individuals. The adaptive immune system, particularly T cells, plays a pivotal role in combating the virus. CD8+ cytotoxic T cells and CD4+ T cells, crucial components of the adaptive immune response, work in harmony to clear the virus and influence the severity of COVID-19 outcomes.
Antigen-Specific T cell Responses to SARS-CoV-2
The adaptive immune response to SARS-CoV-2 is antigen-specific, driven by the recognition of viral epitopes presented by major histocompatibility complex (MHC) molecules. The SARS-CoV-2-specific T cells, predominantly CD4+, recognize epitopes across various viral proteins, with spike antigens dominating CD4+ and CD8+ T cell responses. Following infection or vaccination, these T cells transition into memory T cells, exhibiting robust, long-lasting immunity.
T Cell Cross-Reactivity: An Overview
T cell cross-reactivity can occur through T cell receptor (TCR)-dependent mechanisms, where memory T cells generated in response to one pathogen can recognize and respond to a different, unrelated pathogen. This cross-reactivity has been a subject of extensive research, especially concerning its role in COVID-19 outcomes.
-T Cell Cross-Reactivity and Cross-Protection between SARS-CoV-2 and Other Human Coronaviruses
Early evidence highlighted cross-reactive T cells between SARS-CoV-2 and common human coronaviruses (HCoVs) like OC43, HKU1, NL63, and 229E. These seasonal coronaviruses, prevalent in the human population, share amino acid sequence homology with SARS-CoV-2, leading to the potential for cross-reactive T cell responses. However, debates persist regarding the functional efficacy of these cross-reactive T cells, with studies indicating that low avidity may correlate with severe COVID-19 outcomes.
While cross-reactive T cells from HCoVs may not always offer robust protection, they demonstrate potential in reducing the severity of COVID-19. Notably, cross-reactive T cells against the nucleocapsid protein have shown promise in conferring protection, suggesting a time-dependent effect and paving the way for pan-coronavirus vac cines that leverage non-spike epitopes.
-T Cell Cross-Reactivity between SARS-CoV-2 and Novel Variants
As novel variants of SARS-CoV-2 emerged, concerns arose regarding the potential evasion of pre-existing immunity. While humoral immunity showed decreased efficacy against some variants, memory T cells remained largely unaffected, underscoring their importance in maintaining protection against severe COVID-19 outcomes. Cross-reactive T cells demonstrated resilience against variants, contributing to over 88% protection against severe disease up to 40 weeks after initial infection, regardless of the variant responsible.
T Cell Cross-Reactivity from Different Vaccines or Pathogens
T cell cross-reactivity extends beyond HCoVs, encompassing a diverse range of sources, including vaccines and other pathogens. Exploring cross-reactivity from the Bacillus Calmette–Guérin (BCG) vaccine, influenza, the measles, mumps, and rubella (MMR) vaccine, as well as microbial antigens, reveals a complex interplay of memory T cells and their potential influence on COVID-19 outcomes.
-BCG Vaccine: Early in the pandemic, BCG vaccination demonstrated potential heterologous effects, offering protection against COVID-19. Cross-reactive T cells from BCG vaccination, especially CD4+ and CD8+ memory T cells, exhibited enhanced responses when exposed to SARS-CoV-2, suggesting a potential for improved COVID-19 outcomes.
-Influenza Vaccine: Association between high influenza vaccination coverage and reduced SARS-CoV-2 infection rates prompted investigations into cross-reactive T cells. Shared TCR clonotypes and functional cytokine responses between SARS-CoV-2 and influenza A virus epitopes suggest a potential role for influenza vaccination in influencing the immune response to COVID-19.
-MMR Vaccine: Studies linking the MMR vaccine to better COVID-19 outcomes revealed shared TCR clonotypes with SARS-CoV-2-vaccinated or convalescent individuals. Sequence homologies between MMR surface proteins and the SARS-CoV-2 spike further supported the notion of cross-reactive T cell responses contributing to cross-protection.
-Microbial Antigens: Cross-reactive memory T cells originating from exposure to microbial antigens, both pathogenic and commensal, exhibited homologies with SARS-CoV-2 epitopes. This opens avenues for exploring the contribution of unrelated pathogens to the overall cross-reactive T cell response in COVID-19.
Conclusions and Future Directions
The landscape of T cell cross-reactivity in the context of COVID-19 is dynamic and multifaceted. While evidence suggests the presence of cross-reactive T cells from various sources, further research is essential to unravel their precise impact on clinical outcomes. Understanding the correlation between cross-reactive T cells and protection against severe COVID-19, as well as elucidating the interplay with other immune cells, remains crucial. As the scientific community continues to explore these avenues, the insights gained may contribute to more effective strategies for combating not only SARS-CoV-2 but also potential future coronaviruses.
The study findings were published in the peer reviewed journal: Biomedicines.

 www.mdpi.com
www.mdpi.com
Influence Of Cross-Reactive T Cells In SARS-CoV-2 Infections
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 05, 2024
In the ongoing fight against the COVID-19 pandemic, understanding the intricacies of the immune response has become paramount. One fascinating aspect under intense scrutiny is the role of T cell cross-reactivity – a phenomenon where pre-existing memory T cells, generated in response to diverse infections or vaccinations, exhibit the ability to recognize and mount a response against SARS-CoV-2. This COVID-19 News report delves into the intricate world of T cell cross-reactivity, shedding light on its mechanisms, impact on COVID-19 outcomes, and potential for cross-protection based on a study by researchers from School of Clinical Sciences, Monash University-Australia.
Mechanism of TCR-dependent T cell cross-reactivity with SARS-CoV-2
Adaptive Immune Response to SARS-CoV-2
The Betacoronavirus SARS-CoV-2, responsible for COVID-19, triggers a sophisticated immune response in infected individuals. The adaptive immune system, particularly T cells, plays a pivotal role in combating the virus. CD8+ cytotoxic T cells and CD4+ T cells, crucial components of the adaptive immune response, work in harmony to clear the virus and influence the severity of COVID-19 outcomes.
Antigen-Specific T cell Responses to SARS-CoV-2
The adaptive immune response to SARS-CoV-2 is antigen-specific, driven by the recognition of viral epitopes presented by major histocompatibility complex (MHC) molecules. The SARS-CoV-2-specific T cells, predominantly CD4+, recognize epitopes across various viral proteins, with spike antigens dominating CD4+ and CD8+ T cell responses. Following infection or vaccination, these T cells transition into memory T cells, exhibiting robust, long-lasting immunity.
T Cell Cross-Reactivity: An Overview
T cell cross-reactivity can occur through T cell receptor (TCR)-dependent mechanisms, where memory T cells generated in response to one pathogen can recognize and respond to a different, unrelated pathogen. This cross-reactivity has been a subject of extensive research, especially concerning its role in COVID-19 outcomes.
-T Cell Cross-Reactivity and Cross-Protection between SARS-CoV-2 and Other Human Coronaviruses
Early evidence highlighted cross-reactive T cells between SARS-CoV-2 and common human coronaviruses (HCoVs) like OC43, HKU1, NL63, and 229E. These seasonal coronaviruses, prevalent in the human population, share amino acid sequence homology with SARS-CoV-2, leading to the potential for cross-reactive T cell responses. However, debates persist regarding the functional efficacy of these cross-reactive T cells, with studies indicating that low avidity may correlate with severe COVID-19 outcomes.
While cross-reactive T cells from HCoVs may not always offer robust protection, they demonstrate potential in reducing the severity of COVID-19. Notably, cross-reactive T cells against the nucleocapsid protein have shown promise in conferring protection, suggesting a time-dependent effect and paving the way for pan-coronavirus vac cines that leverage non-spike epitopes.
-T Cell Cross-Reactivity between SARS-CoV-2 and Novel Variants
As novel variants of SARS-CoV-2 emerged, concerns arose regarding the potential evasion of pre-existing immunity. While humoral immunity showed decreased efficacy against some variants, memory T cells remained largely unaffected, underscoring their importance in maintaining protection against severe COVID-19 outcomes. Cross-reactive T cells demonstrated resilience against variants, contributing to over 88% protection against severe disease up to 40 weeks after initial infection, regardless of the variant responsible.
T Cell Cross-Reactivity from Different Vaccines or Pathogens
T cell cross-reactivity extends beyond HCoVs, encompassing a diverse range of sources, including vaccines and other pathogens. Exploring cross-reactivity from the Bacillus Calmette–Guérin (BCG) vaccine, influenza, the measles, mumps, and rubella (MMR) vaccine, as well as microbial antigens, reveals a complex interplay of memory T cells and their potential influence on COVID-19 outcomes.
-BCG Vaccine: Early in the pandemic, BCG vaccination demonstrated potential heterologous effects, offering protection against COVID-19. Cross-reactive T cells from BCG vaccination, especially CD4+ and CD8+ memory T cells, exhibited enhanced responses when exposed to SARS-CoV-2, suggesting a potential for improved COVID-19 outcomes.
-Influenza Vaccine: Association between high influenza vaccination coverage and reduced SARS-CoV-2 infection rates prompted investigations into cross-reactive T cells. Shared TCR clonotypes and functional cytokine responses between SARS-CoV-2 and influenza A virus epitopes suggest a potential role for influenza vaccination in influencing the immune response to COVID-19.
-MMR Vaccine: Studies linking the MMR vaccine to better COVID-19 outcomes revealed shared TCR clonotypes with SARS-CoV-2-vaccinated or convalescent individuals. Sequence homologies between MMR surface proteins and the SARS-CoV-2 spike further supported the notion of cross-reactive T cell responses contributing to cross-protection.
-Microbial Antigens: Cross-reactive memory T cells originating from exposure to microbial antigens, both pathogenic and commensal, exhibited homologies with SARS-CoV-2 epitopes. This opens avenues for exploring the contribution of unrelated pathogens to the overall cross-reactive T cell response in COVID-19.
Conclusions and Future Directions
The landscape of T cell cross-reactivity in the context of COVID-19 is dynamic and multifaceted. While evidence suggests the presence of cross-reactive T cells from various sources, further research is essential to unravel their precise impact on clinical outcomes. Understanding the correlation between cross-reactive T cells and protection against severe COVID-19, as well as elucidating the interplay with other immune cells, remains crucial. As the scientific community continues to explore these avenues, the insights gained may contribute to more effective strategies for combating not only SARS-CoV-2 but also potential future coronaviruses.
The study findings were published in the peer reviewed journal: Biomedicines.

The Influence of Cross-Reactive T Cells in COVID-19
Memory T cells form from the adaptive immune response to historic infections or vaccinations. Some memory T cells have the potential to recognise unrelated pathogens like severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and generate cross-reactive immune responses. Notably, such T...
Heliobas Disciple
TB Fanatic

JN.1’s rock-and-roll party | Voice for Science and Solidarity
This prevention of trans infection protects C-19 vaccinees from severe C-19 disease caused by highly infectious Omicron descendants. Interes
 www.voiceforscienceandsolidarity.org
www.voiceforscienceandsolidarity.org
JN.1’s rock-and-roll party
By Geert Vanden Bossche
March 4, 2024
JN.1’s rock-and-roll party results in an accumulation of various mutations, preparing the spike protein to trigger steric immune evasion. This evolutionary shift poses a formidable threat to public health.
Currently circulating JN.1 clade lineages are highly infectious, primarily spreading through asymptomatically infected Covid-19 (C-19) vaccinees. This has led to sustained high viral infection rates, despite the relatively low mutation rate of SARS-CoV-2 (SC-2). Simultaneously, polyreactive, nonneutralizing IgM Abs (PNNAbs) in C-19 vaccinees are hindering trans infection at the lower respiratory tract.
This prevention of trans infection protects C-19 vaccinees from severe C-19 disease caused by highly infectious Omicron descendants. Interestingly, these are the same antibodies (Abs) that previously contributed to the enhanced infectiousness of early Omicron variants at the level of the upper respiratory tract. These PNNAbs come to bear in the presence of high titers of poorly neutralizing (i.e., low affinity) Abs (Infection-enhancing anti-SARS-CoV-2 antibodies recognize both the original Wuhan/D614G strain and Delta variants. A potential risk for mass vaccination? - PubMed). PNNAbs are presumably produced by B cells lacking memory, and titers sufficient to inhibit SC-2 virulence can therefore only be sustained for as long as the levels of the poorly neutralizing Abs remain high enough to stimulate their production. Consequently, a significant decline in the titers of these poorly neutralizing Abs automatically implies a waning of the PNNAbs. When the concentration of the latter falls below a minimal threshold for virulence inhibition, they exert suboptimal immune pressure on a small antigenic site (so-called ‘enhancing site’) comprised within the N-terminal domain of the spike (S) protein (S-NTD) to which these Abs attach upon recognizing viral particles adsorbed to migratory dendritic cells (The Inescapable Immune Escape Pandemic chapter 6.1).
Suboptimal immune pressure, concentrated on a small antigenic site and occurring collectively within a highly C-19 vaccinated population, causes a high level of immune selection pressure on the virus. This immune selection pressure is not variant-specific, as the targeted antigenic site within the S-NTD is highly conserved among all SC-2 variants. A high infection rate combined with high and widespread variant-nonspecific immune selection pressure on viral (trans) infectiousness explains why many immune escape variants are now rapidly emerging, co-circulating and being transmitted. Competition between a multitude of selected immune escape variants reduces the chance that any specific mutation is transmitted. This situation also enables the virus to accumulate multiple genetic changes during the viral transmission chain, facilitating reshuffling of the amino acid composition of the S protein to selectively accommodate a particular set of site-specific O-glycosylations on the S protein. The targeted change in the S glycosylation profile is likely to cause steric hindrance in the attachment of the virulence-inhibiting Abs to dendritic cell-tethered virions while preserving their fusogenic capacity (Geert Vanden Bossche Predictions on evolution Covid 19 pandemic [UPDATE May 2022] | Voice for Science and Solidarity). Mutations enabling the accommodation of such a specific glycosylation pattern would allow the newly emerging variant to lift the blockade on viral virulence in C-19 vaccinees and thereby evade immune protection from severe illness.
Reports of spectacular mutations are currently accumulating. These mutations are not limited to the S protein but also affect other viral proteins involved in viral reproduction, clearance of viral-infected cells, and even cell metabolic processes, including those that regulate post-translational glycosylation during processing of viral glycoproteins in virus-infected cells. On the other hand, shifts in the distribution of distinct O-linked sugars may already occur as a direct consequence of amino acid mutations (The Inescapable Immune Escape Pandemic chapter 3.4.1).
Given that the S protein is responsible for viral (trans)infectiousness and is, therefore, indispensable for initiating the virus reproduction cycle at the upper and/ or lower respiratory tract, it is not surprising that variants escaping Abs targeting the S protein have a much higher potential for successful transmission compared to variants harboring mutations in proteins involved in other stages of the viral lifecycle. It is therefore reasonable to assume that the transformative mutation that will ultimately unleash the virus’s virulence in highly C-19 vaccinated populations will occur in/ on its S protein.
In conclusion: The virus is now rapidly accruing substantial genetic diversity to accommodate a new, sweet, but unexpected, ally that will give it a new face, one that eludes recognition of the immune subversive mutation by the immune systems of numerous fully vaccinated individuals and likely unleashes the virus’s full virulence.
- Society in highly C-19 vaccinated countries will be caught off guard!-
Heliobas Disciple
TB Fanatic
I'm posting this seemingly unrelated to Covid article because of course the one cause that should be mentioned as contributing to this new health crisis isn't mentioned or considered. As Dr. McMillan calls it - the elephant in the room....

 www.dailymail.co.uk
(fair use applies)
www.dailymail.co.uk
(fair use applies)
Why ARE so many young people having heart attacks? They had seemingly healthy lifestyles... but all these people suffered heart problems
By Cara Lee
Published: 11:58 EST, 4 March 2024 | Updated: 12:18 EST, 4 March 2024
Loading up his car before a football game in September, Dave White waved goodbye to his partner, Vicky, and two young sons as he did every week — with little idea that his life was about to change dramatically.
A short time later, 30 minutes into the game, the 31-year-old had a heart attack on the pitch.
He’d had no pain or other symptoms beforehand and always considered himself to be healthy and active, walking daily and refereeing football matches once or twice a week.
Yet Dave, from Newport in Shropshire, is not alone.
Experts report a worrying rise in the number of under-40s in the UK having heart attacks.
Dave, a father of two, had no pain or other symptoms beforehand and always considered himself to be healthy and active
A heart attack is caused by a sudden loss of blood flow to part of the heart, usually due to a coronary artery becoming blocked. (By contrast, a cardiac arrest, which Dave also experienced, is when the heart suddenly stops pumping due to a dangerous abnormal heart rhythm.)
‘Between 10 to 20 per cent of my heart attack patients are now under the age of 40,’ says Dr Martin Lowe, a consultant cardiologist at St Bartholomew’s Hospital and The Portland Hospital, both in London.
‘In the US, data shows around one in five heart attack patients is under 40 and we’re catching up in the UK.
‘When I was a junior doctor it was extremely rare to see young people — most patients were smokers in their 50s and 60s.’
Dr Joe Mills, a consultant cardiologist at Liverpool Heart and Chest Hospital, adds: ‘We have really noticed the trend for younger people from mid-20s upwards having heart attacks in the past five years in particular.
‘Now as a cardiologist, you wouldn’t even raise your eyebrows when seeing someone in their late 30s — it’s becoming fairly typical, which is frightening.’
So what’s causing the rise in heart attacks in younger people?
A number of factors are to blame, including poor diet and obesity, a sedentary lifestyle, an increase in the number of young people developing type 2 diabetes (which is associated with thicker and stickier blood which raises the risk of blood clots and, in turn, heart attacks), smoking and alcohol, says Dr Lowe.
Obesity often leads to high blood pressure, which can put extra strain on the arteries and heart, and sleep apnoea (disordered patterns of breathing at night that cause you to temporarily stop breathing) can both also lead to blood clots forming.
Another main cause is stress, as Dr Lowe explains: ‘Generally we all live with stress, but it can trigger a heart attack or change in heart rhythm in some people and not others. I’ve seen a huge increase in heart rhythm problems due to stress.’
Professor Thomas Lüscher, a consultant cardiologist at Royal Brompton and Harefield Hospitals in London, says stress activates the sympathetic nervous system, associated with ‘fight or flight’ responses, and this increases our heart rate and can cause the major coronary arteries to contract.
This, in turn, can cause plaque (a substance made of fat and cholesterol which builds up inside the arteries) to rupture, triggering clots to form inside the artery. As the clot grows, it can block blood flow and lead to a heart attack. Dave believes his attack was caused by stress related to his job looking after young people at a children’s care home, and high cholesterol levels that he didn’t know he had.
‘The month before the heart attack, the pressures of my job were getting to me more than they usually do, to the point where I broke down after a shift and was on the verge of resigning,’ he says.
‘The teenagers we look after can have complex needs, so the work can be unpredictable. It was a stressful time.’
As for the day of his heart attack, he says that it had been ‘just a normal day, I’d walked the dog and then I went to referee some football matches — I was feeling fine. The last thing I remember was being on the pitch . . . and then I woke up in hospital five days later’.
Other people at the match later told Dave that he fell over and appeared to have a seizure (this can occur when the brain doesn’t get enough oxygen).
Bystanders gave him CPR and called an ambulance. The paramedics gave him an ECG (an electrocardiogram, a test that records the electrical activity of the heart), which indicated he had a blockage in a coronary artery.
In hospital he was put in an induced coma to protect his brain and allow it to heal after it had been deprived of oxygen. He then had a stent (a short mesh tube) inserted into his left anterior descending artery — the largest artery in the heart — which a scan had revealed was blocked.
‘I was so confused as to why this happened at my age,’ says Dave.
‘I’ve always been active — I walk the dog every day and referee at football weekly without getting breathless.
‘I don’t smoke and hardly drink. I am a bit overweight — maybe by around 2st — but it still didn’t make sense.’
Further tests revealed that despite having no symptoms or history of heart problems in his family, Dave has high cholesterol levels (roughly 8 mmol/L — they should be below five), which raises the risk of heart attacks.
‘My follow-up appointment is this month, and I have so many unanswered questions — such as why do I have high cholesterol,’ he says.
Dave is currently unable to return to his job because the medication he’s been taking since the heart attack (statins, beta blockers, aspirin and blood pressure tablets) have caused side-effects such as breathlessness and abdominal discomfort.
‘Now I’m trying to take better care of myself by eating more healthily and going for longer walks with the dog.
‘Vicky [33, a veterinary nurse] and my sons Harvey, six, and Archie, four, mean everything to me and I want to make sure I’m around for a long time.’ Young people who have heart attacks often have worse outcomes, says Dr Lowe — this is simply because they do not consider they could be having a heart attack and so don’t get the treatment — such as a stent placed in the blocked artery to open it up — quickly enough to minimise long-term heart damage.
A delay in diagnosis raises the risk of a future, bigger and fatal heart attack (subsequent heart attacks are usually more severe while one in three heart attacks is fatal), or heart failure (when the heart cannot pump blood around the body properly), adds Dr Mills.
‘If you’re 35 and living with heart failure, it’s devastating and your life expectancy is dramatically reduced, so it’s a pretty disastrous outcome at that sort of age.’
If someone has chest pain that could be a sign of a heart attack, they should be seen within 30 minutes to give them the greatest chance of a full recovery and restoring normal circulation, advises Dr Lowe.
Heart muscle cells deprived of oxygen can survive if blood flow is restored within 30 minutes; beyond that point, the cells die and are replaced with scar tissue.
‘Younger people almost always fail to recognise symptoms,’ says Dr Mills. ‘Unfortunately, many think they have indigestion when it’s actually a heart attack — they can feel very similar.’
So how can you tell the difference between indigestion or a heart attack?
Dr Lowe says anyone who has never had indigestion before should not assume it is causing their pain, especially if they have any risk factors for heart attack.
‘If symptoms [usually discomfort anywhere above the diaphragm, but most commonly the chest, arms, back, neck or jaw] come on suddenly and last for more than 30 minutes, seem “unusual” or there’s no obvious reason to suspect indigestion — for example you haven’t eaten spicy food or consumed more alcohol than normal — then do not put these symptoms down to indigestion and consider the possibility of a more serious diagnosis such as a heart attack,’ he says.
It’s also important for people with heart-related risk factors, or those with a strong family of heart disease, to get their blood pressure and cholesterol checked — around one in 250 people has a genetic condition which causes very high levels of cholesterol unrelated to diet, known as familial hypercholesterolaemia (FH).
(Dave is currently waiting for an appointment to assess whether or not he has FH.)
‘A lot of people unknowingly have high blood pressure or cholesterol as they don’t have symptoms — and we don’t systematically look for it under the age of 40,’ says Dr Mills.
People of certain ethnicities, particularly those from South Asian countries, are more likely to have heart attacks at a younger age, says Professor Lüscher.
‘They are genetically more likely to be obese, get type 2 diabetes and high blood pressure when they are exposed to a Western lifestyle,’ he explains.
But it’s not just the general public that need to be aware of the risk of heart attack in younger people, many health professionals also don’t recognise the signs, adds Dr Mills.
This leads to people with chest pain being sent home from A&E, only for them to have a major heart attack within a day or two, he adds.
‘A lot of effort has previously been put into making sure healthcare professionals don’t dismiss women with suspected heart attacks, because traditionally heart attacks were thought to affect men — but now we’re getting to the same stage with not dismissing the under-40s.’
And younger women face risk linked to hormones
Another factor for young women in particular is the risk of spontaneous coronary artery dissection (SCAD), where a bruise or tear develops in a coronary artery which cuts off blood flow and results in a heart attack.
This is impossible to predict or prevent.
It is thought that four people a day in the UK have a heart attack due to SCAD, but they don’t have the usual risk factors associated with heart disease and the condition is not fully understood.
As 90 per cent of those affected are women, particularly during pregnancy, after childbirth or around the menopause, fluctuating levels of female sex hormones are thought to play a role in the condition.
Victoria Warnes, 42, from Maidenhead, Berkshire, thought she had pulled a muscle when she experienced chest pain while out jogging six weeks after giving birth to her second child, Wills, in 2017.
‘It was really painful but it felt similar to when I had pulled a chest muscle in my 20s playing tennis,’ says Victoria, who also has a daughter, Olivia, nine.
But the chest pain was actually a sign of a SCAD, which had blocked her main coronary artery by 97 per cent.
Four days later, when the pain worsened and climbing the stairs made her breathless, she went to A&E — where she had an X-ray and ECG. ‘I was a fit 35-year-old, so they were scratching their heads and couldn’t find anything wrong, so I went home and wasn’t given any advice.’
The next morning, becoming more concerned about the increasing discomfort as it wasn’t normal for her, Victoria managed to get a private appointment with a cardiologist — a CT scan showed the severe blockage in her artery and she was rushed to hospital to have a stent fitted to allow blood to pass through her artery. ‘It was very traumatic,’ she says. ‘I was in complete disbelief and all I could think about were the children.
‘Mentally, I was totally broken afterwards — I was so scared it would happen again.’ Victoria believes stress played a part in her SCAD.
‘I was stressed because my husband Rich [44, a business architect] was away for work and I was looking after a newborn and toddler alone, hardly sleeping, and still recovering from a Caesarean section,’ she recalls.
Victoria had a stressful job at an advertising agency until maternity leave, but since the heart attack she has made big changes.
‘When I was having the stent put in, I promised myself I would reduce the stresses I can control — working crazy hours and commuting into London was one of them,’ explains Victoria, who now has annual appointments to monitor her heart.
She left her job and set up Our Baby Club, antenatal classes which focus on parental wellbeing.
‘It was a gift in the end because if it hadn’t happened, I’d still be burning myself into the ground,’ she says.
I run marathons, never smoke or drink - so why me?
Dr Salman Uddin, 38, a GP, lives in Ilford, with his wife Rumana, 37, also a GP, and their two young children.
He says: 'I had never had any signs of heart problems — in fact, I considered myself fit and healthy. I regularly ran — I’ve completed three London marathons — had never smoked and didn’t drink alcohol.
'Then, one weekend in July 2020, I went for a 10K run. I hadn’t been running for a few weeks due to the Covid lockdown rules and so I paced myself.
'It went smoothly, though I was slightly slower than usual. I figured this was because I hadn’t run in a while.
'When I got home, I went upstairs to shower, and as I got undressed noticed I was sweating profusely. Rumana came in and saw I looked so wet, she thought I’d already showered! Then I developed a pain in my chest, which quickly spread to my neck.
'I wondered whether the run had triggered indigestion, so I asked Rumana for a Gaviscon tablet, but she ignored me and called 999.
'By this time I was sitting on the floor, pain racking my body. Our baby daughter was on the bed gurgling away; she smiled at me and for a moment I was distracted but then the pain hit me in a sudden wave, spreading all down my arm, across my chest and neck.
'When the paramedics arrived, they seemed jovial and didn’t mention "heart attack", presumably because I was young and fit. I was able to walk to the ambulance with them, where they hooked me up to an ECG to check my heart activity — and then their faces dropped. Suddenly I was being blue-lit to St Barts Hospital in London.
'By now the pain was greater, so they gave me morphine as well as aspirin to thin the blood.
'In hospital I was whisked through for an angiogram — a sort of X-ray on the heart and arteries around it — and it confirmed I had a blockage in an artery. I’d experienced a heart attack.
'I was shocked, as I’d never had any symptoms, nor did I have any of the obvious risk factors: I was not a smoker, a drinker, nor diabetic, I ran regularly and there was no family history of heart disease. They said it was "one of those things" — there was no obvious cause. The same day, I was taken to the operating theatre, where a cardiologist inserted a stent to open the blocked artery. I was kept in hospital for three days. I was given medication to prevent future attacks, including aspirin, clopidogrel, lansoprazole and candesartan.
'Afterwards life seemed surreal. I was in shock that this had happened to me — a person who is not a traditional heart attack patient.
'I spend my life advising patients on losing weight and staying healthy, and now I’d had a heart attack; clearly sometimes they happen despite your best efforts to stay healthy.
'Now I’m back to running and eating healthily — but I’m telling my story to warn others not to ignore signs of a heart attack, even if you are young, sporty and seemingly healthy.'

Why ARE so many young people having heart attacks?
Dave White waved goodbye to his partner, Vicky, and two young sons with little idea that his life was about to change dramatically. A short time later, the 31-year-old had a heart attack on the pitch.
Why ARE so many young people having heart attacks? They had seemingly healthy lifestyles... but all these people suffered heart problems
By Cara Lee
Published: 11:58 EST, 4 March 2024 | Updated: 12:18 EST, 4 March 2024
Loading up his car before a football game in September, Dave White waved goodbye to his partner, Vicky, and two young sons as he did every week — with little idea that his life was about to change dramatically.
A short time later, 30 minutes into the game, the 31-year-old had a heart attack on the pitch.
He’d had no pain or other symptoms beforehand and always considered himself to be healthy and active, walking daily and refereeing football matches once or twice a week.
Yet Dave, from Newport in Shropshire, is not alone.
Experts report a worrying rise in the number of under-40s in the UK having heart attacks.
Dave, a father of two, had no pain or other symptoms beforehand and always considered himself to be healthy and active
A heart attack is caused by a sudden loss of blood flow to part of the heart, usually due to a coronary artery becoming blocked. (By contrast, a cardiac arrest, which Dave also experienced, is when the heart suddenly stops pumping due to a dangerous abnormal heart rhythm.)
‘Between 10 to 20 per cent of my heart attack patients are now under the age of 40,’ says Dr Martin Lowe, a consultant cardiologist at St Bartholomew’s Hospital and The Portland Hospital, both in London.
‘In the US, data shows around one in five heart attack patients is under 40 and we’re catching up in the UK.
‘When I was a junior doctor it was extremely rare to see young people — most patients were smokers in their 50s and 60s.’
Dr Joe Mills, a consultant cardiologist at Liverpool Heart and Chest Hospital, adds: ‘We have really noticed the trend for younger people from mid-20s upwards having heart attacks in the past five years in particular.
‘Now as a cardiologist, you wouldn’t even raise your eyebrows when seeing someone in their late 30s — it’s becoming fairly typical, which is frightening.’
So what’s causing the rise in heart attacks in younger people?
A number of factors are to blame, including poor diet and obesity, a sedentary lifestyle, an increase in the number of young people developing type 2 diabetes (which is associated with thicker and stickier blood which raises the risk of blood clots and, in turn, heart attacks), smoking and alcohol, says Dr Lowe.
Obesity often leads to high blood pressure, which can put extra strain on the arteries and heart, and sleep apnoea (disordered patterns of breathing at night that cause you to temporarily stop breathing) can both also lead to blood clots forming.
Another main cause is stress, as Dr Lowe explains: ‘Generally we all live with stress, but it can trigger a heart attack or change in heart rhythm in some people and not others. I’ve seen a huge increase in heart rhythm problems due to stress.’
Professor Thomas Lüscher, a consultant cardiologist at Royal Brompton and Harefield Hospitals in London, says stress activates the sympathetic nervous system, associated with ‘fight or flight’ responses, and this increases our heart rate and can cause the major coronary arteries to contract.
This, in turn, can cause plaque (a substance made of fat and cholesterol which builds up inside the arteries) to rupture, triggering clots to form inside the artery. As the clot grows, it can block blood flow and lead to a heart attack. Dave believes his attack was caused by stress related to his job looking after young people at a children’s care home, and high cholesterol levels that he didn’t know he had.
‘The month before the heart attack, the pressures of my job were getting to me more than they usually do, to the point where I broke down after a shift and was on the verge of resigning,’ he says.
‘The teenagers we look after can have complex needs, so the work can be unpredictable. It was a stressful time.’
As for the day of his heart attack, he says that it had been ‘just a normal day, I’d walked the dog and then I went to referee some football matches — I was feeling fine. The last thing I remember was being on the pitch . . . and then I woke up in hospital five days later’.
Other people at the match later told Dave that he fell over and appeared to have a seizure (this can occur when the brain doesn’t get enough oxygen).
Bystanders gave him CPR and called an ambulance. The paramedics gave him an ECG (an electrocardiogram, a test that records the electrical activity of the heart), which indicated he had a blockage in a coronary artery.
In hospital he was put in an induced coma to protect his brain and allow it to heal after it had been deprived of oxygen. He then had a stent (a short mesh tube) inserted into his left anterior descending artery — the largest artery in the heart — which a scan had revealed was blocked.
‘I was so confused as to why this happened at my age,’ says Dave.
‘I’ve always been active — I walk the dog every day and referee at football weekly without getting breathless.
‘I don’t smoke and hardly drink. I am a bit overweight — maybe by around 2st — but it still didn’t make sense.’
Further tests revealed that despite having no symptoms or history of heart problems in his family, Dave has high cholesterol levels (roughly 8 mmol/L — they should be below five), which raises the risk of heart attacks.
‘My follow-up appointment is this month, and I have so many unanswered questions — such as why do I have high cholesterol,’ he says.
Dave is currently unable to return to his job because the medication he’s been taking since the heart attack (statins, beta blockers, aspirin and blood pressure tablets) have caused side-effects such as breathlessness and abdominal discomfort.
‘Now I’m trying to take better care of myself by eating more healthily and going for longer walks with the dog.
‘Vicky [33, a veterinary nurse] and my sons Harvey, six, and Archie, four, mean everything to me and I want to make sure I’m around for a long time.’ Young people who have heart attacks often have worse outcomes, says Dr Lowe — this is simply because they do not consider they could be having a heart attack and so don’t get the treatment — such as a stent placed in the blocked artery to open it up — quickly enough to minimise long-term heart damage.
A delay in diagnosis raises the risk of a future, bigger and fatal heart attack (subsequent heart attacks are usually more severe while one in three heart attacks is fatal), or heart failure (when the heart cannot pump blood around the body properly), adds Dr Mills.
‘If you’re 35 and living with heart failure, it’s devastating and your life expectancy is dramatically reduced, so it’s a pretty disastrous outcome at that sort of age.’
If someone has chest pain that could be a sign of a heart attack, they should be seen within 30 minutes to give them the greatest chance of a full recovery and restoring normal circulation, advises Dr Lowe.
Heart muscle cells deprived of oxygen can survive if blood flow is restored within 30 minutes; beyond that point, the cells die and are replaced with scar tissue.
‘Younger people almost always fail to recognise symptoms,’ says Dr Mills. ‘Unfortunately, many think they have indigestion when it’s actually a heart attack — they can feel very similar.’
So how can you tell the difference between indigestion or a heart attack?
Dr Lowe says anyone who has never had indigestion before should not assume it is causing their pain, especially if they have any risk factors for heart attack.
‘If symptoms [usually discomfort anywhere above the diaphragm, but most commonly the chest, arms, back, neck or jaw] come on suddenly and last for more than 30 minutes, seem “unusual” or there’s no obvious reason to suspect indigestion — for example you haven’t eaten spicy food or consumed more alcohol than normal — then do not put these symptoms down to indigestion and consider the possibility of a more serious diagnosis such as a heart attack,’ he says.
It’s also important for people with heart-related risk factors, or those with a strong family of heart disease, to get their blood pressure and cholesterol checked — around one in 250 people has a genetic condition which causes very high levels of cholesterol unrelated to diet, known as familial hypercholesterolaemia (FH).
(Dave is currently waiting for an appointment to assess whether or not he has FH.)
‘A lot of people unknowingly have high blood pressure or cholesterol as they don’t have symptoms — and we don’t systematically look for it under the age of 40,’ says Dr Mills.
People of certain ethnicities, particularly those from South Asian countries, are more likely to have heart attacks at a younger age, says Professor Lüscher.
‘They are genetically more likely to be obese, get type 2 diabetes and high blood pressure when they are exposed to a Western lifestyle,’ he explains.
But it’s not just the general public that need to be aware of the risk of heart attack in younger people, many health professionals also don’t recognise the signs, adds Dr Mills.
This leads to people with chest pain being sent home from A&E, only for them to have a major heart attack within a day or two, he adds.
‘A lot of effort has previously been put into making sure healthcare professionals don’t dismiss women with suspected heart attacks, because traditionally heart attacks were thought to affect men — but now we’re getting to the same stage with not dismissing the under-40s.’
And younger women face risk linked to hormones
Another factor for young women in particular is the risk of spontaneous coronary artery dissection (SCAD), where a bruise or tear develops in a coronary artery which cuts off blood flow and results in a heart attack.
This is impossible to predict or prevent.
It is thought that four people a day in the UK have a heart attack due to SCAD, but they don’t have the usual risk factors associated with heart disease and the condition is not fully understood.
As 90 per cent of those affected are women, particularly during pregnancy, after childbirth or around the menopause, fluctuating levels of female sex hormones are thought to play a role in the condition.
Victoria Warnes, 42, from Maidenhead, Berkshire, thought she had pulled a muscle when she experienced chest pain while out jogging six weeks after giving birth to her second child, Wills, in 2017.
‘It was really painful but it felt similar to when I had pulled a chest muscle in my 20s playing tennis,’ says Victoria, who also has a daughter, Olivia, nine.
But the chest pain was actually a sign of a SCAD, which had blocked her main coronary artery by 97 per cent.
Four days later, when the pain worsened and climbing the stairs made her breathless, she went to A&E — where she had an X-ray and ECG. ‘I was a fit 35-year-old, so they were scratching their heads and couldn’t find anything wrong, so I went home and wasn’t given any advice.’
The next morning, becoming more concerned about the increasing discomfort as it wasn’t normal for her, Victoria managed to get a private appointment with a cardiologist — a CT scan showed the severe blockage in her artery and she was rushed to hospital to have a stent fitted to allow blood to pass through her artery. ‘It was very traumatic,’ she says. ‘I was in complete disbelief and all I could think about were the children.
‘Mentally, I was totally broken afterwards — I was so scared it would happen again.’ Victoria believes stress played a part in her SCAD.
‘I was stressed because my husband Rich [44, a business architect] was away for work and I was looking after a newborn and toddler alone, hardly sleeping, and still recovering from a Caesarean section,’ she recalls.
Victoria had a stressful job at an advertising agency until maternity leave, but since the heart attack she has made big changes.
‘When I was having the stent put in, I promised myself I would reduce the stresses I can control — working crazy hours and commuting into London was one of them,’ explains Victoria, who now has annual appointments to monitor her heart.
She left her job and set up Our Baby Club, antenatal classes which focus on parental wellbeing.
‘It was a gift in the end because if it hadn’t happened, I’d still be burning myself into the ground,’ she says.
I run marathons, never smoke or drink - so why me?
Dr Salman Uddin, 38, a GP, lives in Ilford, with his wife Rumana, 37, also a GP, and their two young children.
He says: 'I had never had any signs of heart problems — in fact, I considered myself fit and healthy. I regularly ran — I’ve completed three London marathons — had never smoked and didn’t drink alcohol.
'Then, one weekend in July 2020, I went for a 10K run. I hadn’t been running for a few weeks due to the Covid lockdown rules and so I paced myself.
'It went smoothly, though I was slightly slower than usual. I figured this was because I hadn’t run in a while.
'When I got home, I went upstairs to shower, and as I got undressed noticed I was sweating profusely. Rumana came in and saw I looked so wet, she thought I’d already showered! Then I developed a pain in my chest, which quickly spread to my neck.
'I wondered whether the run had triggered indigestion, so I asked Rumana for a Gaviscon tablet, but she ignored me and called 999.
'By this time I was sitting on the floor, pain racking my body. Our baby daughter was on the bed gurgling away; she smiled at me and for a moment I was distracted but then the pain hit me in a sudden wave, spreading all down my arm, across my chest and neck.
'When the paramedics arrived, they seemed jovial and didn’t mention "heart attack", presumably because I was young and fit. I was able to walk to the ambulance with them, where they hooked me up to an ECG to check my heart activity — and then their faces dropped. Suddenly I was being blue-lit to St Barts Hospital in London.
'By now the pain was greater, so they gave me morphine as well as aspirin to thin the blood.
'In hospital I was whisked through for an angiogram — a sort of X-ray on the heart and arteries around it — and it confirmed I had a blockage in an artery. I’d experienced a heart attack.
'I was shocked, as I’d never had any symptoms, nor did I have any of the obvious risk factors: I was not a smoker, a drinker, nor diabetic, I ran regularly and there was no family history of heart disease. They said it was "one of those things" — there was no obvious cause. The same day, I was taken to the operating theatre, where a cardiologist inserted a stent to open the blocked artery. I was kept in hospital for three days. I was given medication to prevent future attacks, including aspirin, clopidogrel, lansoprazole and candesartan.
'Afterwards life seemed surreal. I was in shock that this had happened to me — a person who is not a traditional heart attack patient.
'I spend my life advising patients on losing weight and staying healthy, and now I’d had a heart attack; clearly sometimes they happen despite your best efforts to stay healthy.
'Now I’m back to running and eating healthily — but I’m telling my story to warn others not to ignore signs of a heart attack, even if you are young, sporty and seemingly healthy.'
Profit of Doom
Dismember
The question should be, “when should I start my early treatment protocol?”I have symptoms. When should I take a test?
Yesterday.
northern watch
TB Fanatic
Chicory
#KeeptheRepublic
Another autoimmune disorder- seems to be a Fauci speciality.

 vigilantnews.com
vigilantnews.com
Published 2 mins ago on March 5, 2024
By vnninfluencers

This article originally appeared on The Epoch Times and was republished with permission.
Guest post by Marina Zhang
Dr. Clarice Saba, an otorhinolaryngologist in Brazil, developed sudden hearing loss in her right ear a week after receiving her first dose of the COVID-19 adenovirus vaccine.
“I did all the exams and could not find any other reason other than because of the shots,” she told The Epoch Times.
Several studies have linked sudden hearing loss to the vaccine, with the most comprehensive study coming from France. Four hundred cases of post-vaccine sudden sensorineural hearing loss were evaluated, with 345 medical reports assessed by two audiology experts for potential causality.
“[Sudden sensorineural hearing loss] after COVID-19 mRNA vaccines are very rare adverse events,” the French authors concluded, adding that these rare adverse events “do not call into question the benefits of mRNA vaccines but deserve to be known given the potentially disabling impact of sudden deafness.”
This assumption is based on the fact that cochlear implants, which mimic the work of a natural cochlea, are highly successful in treating hearing loss.
The cochlea is a highly sensitive part of the ear and can accumulate damage from aging, loud sounds, viral infections, and certain chemicals and medications.
These exposures may restrict oxygen to the blood supply of the cochlea, reduce blood flow, increase oxidative damage, or form lesions in the cochlear tissue.
It is not known how COVID-19 and its vaccines may cause hearing loss. Some studies have proposed that the SARS-CoV-2 virus may replicate in the ears and cause damage to the blood vessels and nerves there. Case studies evaluating hearing problems in COVID-19 patients found inflammation of the inner ears, inflamed cochlea and vestibular nerves, and bleeding of the ears.
The COVID-19 mRNA vaccines induce the body to make COVID-19 spike proteins. Research in animal cochlear cells has shown that the spike protein damages the cochlea. Spike proteins also share structural similarities with over 28 human proteins. Therefore, some studies on hearing loss speculate that proteins in the ears, including within the cochlea, may be structurally similar to spike proteins, leading to autoimmune damage when the body mounts its immune response.
The spike proteins in the COVID-19 vaccines are also prone to causing microclotting, where the blood becomes more viscous and “sludge-like,” according to internal medicine physician Dr. Jordan Vaughn. Viscous blood moves more slowly, reducing oxygen exchange in the blood and leading to stress on the nerves and cells in the ears.
Tinnitus is a much more common and acknowledged adverse effect of the COVID-19 vaccine than some. A well-known case of vaccine-related tinnitus was reported by vaccinologist Dr. Gregory Poland, who developed the condition after getting his second Pfizer dose.
Tinnitus is also strongly linked to hearing loss.
While most patients with tinnitus may not realize signs of hearing loss, around 80 percent to 90 percent have the issue.
Dr. Saba said that many patients with tinnitus may get a normal hearing result when they undergo an automatic hearing test. However, tests for hearing at high frequencies or audiometric hearing tests would reveal that the person has some degree of hearing loss. Studies have shown that the cochlea is also involved in chronic tinnitus.
Due to the link between tinnitus and hearing loss, she sometimes prescribes the same treatment for both conditions.

New Problem Emerges for the COVID Vaccinated
Some studies suggest an autoimmune reaction induced by the spike protein may be to blame.
 vigilantnews.com
vigilantnews.com
New Problem Emerges for the COVID Vaccinated
Some studies suggest an autoimmune reaction induced by the spike protein may be to blame.Published 2 mins ago on March 5, 2024
By vnninfluencers

This article originally appeared on The Epoch Times and was republished with permission.
Guest post by Marina Zhang
Dr. Clarice Saba, an otorhinolaryngologist in Brazil, developed sudden hearing loss in her right ear a week after receiving her first dose of the COVID-19 adenovirus vaccine.
“I did all the exams and could not find any other reason other than because of the shots,” she told The Epoch Times.
Several studies have linked sudden hearing loss to the vaccine, with the most comprehensive study coming from France. Four hundred cases of post-vaccine sudden sensorineural hearing loss were evaluated, with 345 medical reports assessed by two audiology experts for potential causality.
“[Sudden sensorineural hearing loss] after COVID-19 mRNA vaccines are very rare adverse events,” the French authors concluded, adding that these rare adverse events “do not call into question the benefits of mRNA vaccines but deserve to be known given the potentially disabling impact of sudden deafness.”
Accumulated Damage
While the cause of hearing loss is unknown, it is usually assumed to be induced by damage to the cochlea, a fluid-filled, spiral cavity in the inner ear that helps process sounds into electrical signals in the brain.This assumption is based on the fact that cochlear implants, which mimic the work of a natural cochlea, are highly successful in treating hearing loss.
The cochlea is a highly sensitive part of the ear and can accumulate damage from aging, loud sounds, viral infections, and certain chemicals and medications.
These exposures may restrict oxygen to the blood supply of the cochlea, reduce blood flow, increase oxidative damage, or form lesions in the cochlear tissue.
It is not known how COVID-19 and its vaccines may cause hearing loss. Some studies have proposed that the SARS-CoV-2 virus may replicate in the ears and cause damage to the blood vessels and nerves there. Case studies evaluating hearing problems in COVID-19 patients found inflammation of the inner ears, inflamed cochlea and vestibular nerves, and bleeding of the ears.
The COVID-19 mRNA vaccines induce the body to make COVID-19 spike proteins. Research in animal cochlear cells has shown that the spike protein damages the cochlea. Spike proteins also share structural similarities with over 28 human proteins. Therefore, some studies on hearing loss speculate that proteins in the ears, including within the cochlea, may be structurally similar to spike proteins, leading to autoimmune damage when the body mounts its immune response.
The spike proteins in the COVID-19 vaccines are also prone to causing microclotting, where the blood becomes more viscous and “sludge-like,” according to internal medicine physician Dr. Jordan Vaughn. Viscous blood moves more slowly, reducing oxygen exchange in the blood and leading to stress on the nerves and cells in the ears.
Tinnitus and Hearing Loss
Since the pandemic, Dr. Saba has seen a rise in hearing loss and tinnitus.Tinnitus is a much more common and acknowledged adverse effect of the COVID-19 vaccine than some. A well-known case of vaccine-related tinnitus was reported by vaccinologist Dr. Gregory Poland, who developed the condition after getting his second Pfizer dose.
Tinnitus is also strongly linked to hearing loss.
While most patients with tinnitus may not realize signs of hearing loss, around 80 percent to 90 percent have the issue.
Dr. Saba said that many patients with tinnitus may get a normal hearing result when they undergo an automatic hearing test. However, tests for hearing at high frequencies or audiometric hearing tests would reveal that the person has some degree of hearing loss. Studies have shown that the cochlea is also involved in chronic tinnitus.
Due to the link between tinnitus and hearing loss, she sometimes prescribes the same treatment for both conditions.
jward
passin' thru
Jim Ferguson
@JimFergusonUK
Alert: England’s vaccinated population had close to one million deaths in 23 months; unvaccinated population had less than 61,000 deaths over the same period
Shocking data released by the U.K. government shows that over the past two years, the vaccinated population in England has suffered an outrageous number of deaths compared to the unvaccinated population, even though approximately 30 percent of the population has not even had a single dose of the Wuhan coronavirus (COVID-19) vaccine.
According to the U.K. Health Security Agency (UKHSA), by July 2022, 18.9 million people had refused the first dose of the COVID-19 injection, 21.5 million people had refused the second dose of the COVID-19 injection, alongside 2.6 million people who had received the first dose but refused the second, and 30.4 million people had refused the third dose of the COVID-19 injection, alongside 8.9 million people who had received the second dose but refused the third. (Related: CAUGHT: UK hospitals certified pneumonia deaths as COVID deaths to create illusion of pandemic.)
According to the UKHSA's figures, 63.4 million people were eligible for vaccination at that point. Therefore, as of July 2022, 30 percent of England's population remained completely unvaccinated; 34 percent was not double vaccinated; and 50 percent was not triple vaccinated. However, the vaccinated population as a whole accounted for 95 percent of all COVID-19 deaths between January and May 2023, while the unvaccinated population accounted for just five percent.
But it's the fact that these deaths aren't among the one-dose and two-dose vaccinated population that is truly horrifying.
The vast majority are among those vaccinated four times, with this population accounting for 80 percent of all COVID-19 deaths, and 83 percent of all COVID-19 deaths among the vaccinated.
#VaccineInjuries #mRNA #DiedSuddenly #ExcessDaeths #UK

 naturalnews.com
naturalnews.com
@JimFergusonUK
Alert: England’s vaccinated population had close to one million deaths in 23 months; unvaccinated population had less than 61,000 deaths over the same period
Shocking data released by the U.K. government shows that over the past two years, the vaccinated population in England has suffered an outrageous number of deaths compared to the unvaccinated population, even though approximately 30 percent of the population has not even had a single dose of the Wuhan coronavirus (COVID-19) vaccine.
According to the U.K. Health Security Agency (UKHSA), by July 2022, 18.9 million people had refused the first dose of the COVID-19 injection, 21.5 million people had refused the second dose of the COVID-19 injection, alongside 2.6 million people who had received the first dose but refused the second, and 30.4 million people had refused the third dose of the COVID-19 injection, alongside 8.9 million people who had received the second dose but refused the third. (Related: CAUGHT: UK hospitals certified pneumonia deaths as COVID deaths to create illusion of pandemic.)
According to the UKHSA's figures, 63.4 million people were eligible for vaccination at that point. Therefore, as of July 2022, 30 percent of England's population remained completely unvaccinated; 34 percent was not double vaccinated; and 50 percent was not triple vaccinated. However, the vaccinated population as a whole accounted for 95 percent of all COVID-19 deaths between January and May 2023, while the unvaccinated population accounted for just five percent.
But it's the fact that these deaths aren't among the one-dose and two-dose vaccinated population that is truly horrifying.
The vast majority are among those vaccinated four times, with this population accounting for 80 percent of all COVID-19 deaths, and 83 percent of all COVID-19 deaths among the vaccinated.
#VaccineInjuries #mRNA #DiedSuddenly #ExcessDaeths #UK

The world's top new source on natural health - NaturalNews.com
The world's top new source on natural health - NaturalNews.com
Heliobas Disciple
TB Fanatic

House COVID panel subpoenas former NY Gov. Cuomo over nursing home deaths
The House committee investigating the coronavirus pandemic response issued a subpoena Tuesday for former New York Gov. Andrew Cuomo (D) over his alleged failure to cooperate with a probe into the state’s COVID-19 nursing home policies. The House Select Subcommittee on the Coronavirus Pandemic is...
House COVID panel subpoenas former NY Gov. Cuomo over nursing home deaths
Nathaniel Weixel - The Hill
Tue, March 5, 2024, 3:42 PM EST
The House committee investigating the coronavirus pandemic response issued a subpoena Tuesday for former New York Gov. Andrew Cuomo (D) over his alleged failure to cooperate with a probe into the state’s COVID-19 nursing home policies.
The House Select Subcommittee on the Coronavirus Pandemic is demanding Cuomo appear for a closed-door deposition on May 24. Rep. Brad Wenstrup (R-Ohio), the subcommittee’s chairman, has previously requested interviews with former Cuomo administration officials, including former top aide Melissa DeRosa.
Cuomo became a nationally known figure early in the pandemic by conducting daily briefings from Albany, contrasting himself with then-President Trump.
Wenstrup in a statement accused the former governor of stonewalling the investigation and said the panel had been met with months and months of “repeated and unjustified delays.”
The panel has been investigating COVID-19 nursing home policy decisions made by Cuomo and the Democratic leaders of New Jersey and Pennsylvania.
Specifically, the panel is looking into Cuomo’s “must admit” order, which said nursing homes could not turn away patients who tested positive for COVID-19, as long as they were medically stable.
The facilities were also prohibited from requiring hospitalized residents to be tested for the virus before their admission or readmission in nursing homes.
The move was made early in the pandemic and was meant to help relieve overburdened hospitals, which were sending patients elsewhere to help free up capacity.
The virus decimated New York’s nursing homes, killing more than 15,000 people. But multiple investigations into the Cuomo administration’s nursing home policies by the Department of Justice as well as state and local investigators did not lead to any conclusions of wrongdoing.
In early 2021, a report from New York State Attorney General Letitia James found that COVID deaths in New York state had been “undercounted” by as much as 50 percent.
Cuomo resigned in August 2021 amid allegations of sexual harassment and inappropriate behavior, and as criticism of his COVID response mounted.
“Not only did the former Governor put the elderly in harm’s way, but he also attempted to cover-up his failures by hiding the true nursing home death rate,” Wenstrup said in a statement. “It appears that politics, not medicine, was responsible for these decisions. And that while Mr. Cuomo is adept at seeking legal advice, he is not necessarily adept at seeking medical advice.”
Cuomo spokesman Rich Azzopardi said the subpoena is a political attack, and slammed House Republicans for failing to pass a budget or Ukraine aid.
“Instead, they continue to play politics with Covid and weaponize people’s pain and loss of loved ones,” Azzopardi said. “Congress is officially a circus and they are nothing but clowns.”
Wenstrup’s letter describes months of back-and-forth between the committee and Cuomo’s representatives over the past three months, which the Ohio Republican described as stalling attempts.
“It is now clear that your strategy from the beginning has been to delay and undermine our investigation. You have repeatedly and consistently dismissed, deflected, or ignored all questions and requests from the Select Subcommittee related to your handling of nursing homes,” Wenstrup wrote.
Cuomo’s attorney Rita Galvin said the former governor “has been and remains cooperative.” In an attempt to stave off a subpoena, she sent a letter to the panel on Monday proposing four potential dates in August for a voluntary interview.
Heliobas Disciple
TB Fanatic

The Covid-19 pandemic killed off one strain of the flu, and that will change the next vaccines
For ten years, Americans have had access to flu shots that protect against four different strains of the flu—two A strains and two B strains. Starting this fall, however, all the flu shots distributed in the United States will contain only three strains, and the change happened in part because...
The Covid-19 pandemic killed off one strain of the flu, and that will change the next vaccines
Brenda Goodman, CNN
Tue, March 5, 2024, 3:51 PM EST
For 10 years, Americans have had access to flu shots that protect against four strains of the virus: two A strains and two B strains.
Starting this fall, however, all the flu shots distributed in the United States will contain only three strains, and the change happened in part because of Covid-19.
On Tuesday, a panel of experts who advise the US Food and Drug Administration on vaccines voted unanimously to recommend three-strain flu vaccines that will exclude any viruses from B strains that are part of branch of the flu’s family tree called Yamagata.
Yamagata viruses were in decline before the pandemic, and all the precautions that helped people avoid Covid-19 – including masking, staying at home and better ventilation – appear to have finished them off. They haven’t been detected in testing since March 2020.
One Yamagata strain was typically included in each year’s flu shot recipe, so vaccine designers faced a quandary this year: Should they drop the strain from the formula or keep it in, since B-viruses are known to be cagey?
In the 1990s, when Yamagata was in its heyday, another branch of B-strain flu viruses called Victoria was seen only sporadically in testing, but it had a resurgence in the 2000s. What if Yamagata came back after a lengthy absence? It’s not quick or easy to change how flu vaccines are manufactured, and those changes require regulatory review and approval.
In September, the World Health Organization said that “inclusion of the Yamagata-lineage antigens in influenza vaccines is no longer warranted,” and in October, the FDA’s vaccine experts also said the Yamagata strains should be dropped as quickly as possible.
“We’ve been talking about this for four years,” said Dr. Paul Offit, director of the Vaccine Education Center at Children’s Hospital of Philadelphia and a member of the FDA’s Vaccines and Biological Products Advisory Committee, or VRBPAC.
The change is happening faster than expected, said Dr. Arnold Monto, another VRBPAC member. He noted that in October, when the committee first voted to recommend removing Yamagata from flu vaccines, they were told that it might be impossible to exclude it next season because of regulatory red tape.
Dr. Jerry Weir, director of the FDA’s Division of Viral Products, said Tuesday that the agency has been working with manufacturers to get the Yamagata strain out of US vaccines in time for the 2024-25 flu season.
“At this point in time, each of the US influenza vaccine manufacturers have submitted updated regulatory files related to a trivalent influenza vaccine, and approval of all the necessary regulatory submissions is on track for 2024-25” season, he said during the advisory committee’s meeting.
In fact, Weir noted, the US was able to move faster than some other countries because all the vaccine manufacturers already had approvals for trivalent flu vaccines here. It’s taking longer in other parts of the world to make the switch.
For that reason, the committee also voted to recommend a four-strain formula – including one from B/Yamagata – for vaccines that will be manufactured in the US but distributed in other countries.
“And I think we should congratulate both FDA and the manufacturers of making this possible, because the problem seems to be totally logistic,” Weir said.
There are good reasons for dropping the Yamagata strain, Offit said.
“You don’t want to be vaccinating people for something they don’t need,” he said.
There may also be some harms in continuing to include it, said Dr. Jodie Guest, senior vice chair of the Department of Epidemiology at Emory University’s Rollins School of Public Health, who is not a member of the FDA committee.
“Anytime these flu vaccines are being produced, they are – depending on which vaccines you are talking about – using live or attenuated virus, and you do have to grow it,” she said. Growing something in a lab also means it could escape from that lab.
“So while it would be an anticipated, incredibly small risk, there is the possibility you could reintroduce it into the population by having it contained in a vaccine,” Guest said.
Other researchers have pointed out that dropping the Yamagata strain would free up production capacity to increase the number of doses made globally, something that would benefit countries affected by shortages.
In an article on the expected changes published February 28 in the New England Journal of Medicine, Monto, Weir and Dr. Maria Zambon from the UK Health Security Agency said the move opens the door to considering new vaccine formulas.
Since the shot’s B/Victoria and A/H1N1 strains are often more effective than the A/H3N2 component, some experts have suggested doubling the dose of H3N2 or perhaps slipping in a second member of that family.
But as the authors note, any such change would require testing and regulatory approval, and for that reason, it’s not likely we’ll see the return of four-strain flu shots very quickly. Instead, they say, it will be “more of a long-term goal for improving vaccine effectiveness.”
In the meantime, scientists will keep testing flu viruses, just to make sure Yamagata really has been relegated to the history books.
Heliobas Disciple
TB Fanatic
(fair use applies)
Thailand Medical Authorities On Alert As Researcher Claims That New BA.2.87.1 Sub-Lineages Found In Wastewater Samples In South-East Asia
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 06, 2024
Thailand Medical authorities are on alert as a Sri Lankan researcher currently based in Japan has claimed that that the BA.2.87.1 sub-lineages have been detected in wastewater samples in South-East Asia. This is extremely interesting as this is the first time that there is any mention of the detection of the BA.2.87 or its sub-lineages BA.2.87.1 being detected out of South Africa since it was identified in early February 2024.
Dr Leshan Wannigama who had previously completed his PhD at the Chulalongkprn University in Thailand, and currently based in Yamagata Prefectural University of Health Sciences in Japan had posted online that the BA.2.87.1 sub-lineages had been found in waste water samples in South East Asia. He was also involved in waste water monitoring in Bangkok.
View: https://twitter.com/dr_leshan/status/1764186732701094143
He stopped short of identifying which South-East Asia countries in which these sub-lineages had been detected in and also he did not provide any further evidence of his claims but the rest of the ‘variant hunters’ online seem to have agreed with his claims.
Thailand Medical authorities, researchers and doctors have stepped up genomic surveillance in the country and hospitals are closely monitoring the situation. However, to date, there has been no official announcements that the BA.2.87.1 has been detected in the Thailand and it could possibility other South-East Asian countries that he was referring to.
A recent German research has been published as a preprint identifying the properties of this new BA.2.87.1 sub-lineages. Some of the unique properties of the BA.2.87.1 are worrying with implications of possible increased risk of disease severity upon being infected with such sub-lineages!

 www.biorxiv.org
www.biorxiv.org
Interestingly the BA.2.87.1 sub-lineages were detected in waste water samples between December 2023 last week and January 2024 second week in South-East Asia according to Dr Wannigama.
View: https://twitter.com/dr_leshan/status/1764419784345575451
This raises a lot of questions as to whether the BA.2.87 variant originated in South Africa or elsewhere.
Interestingly after the BA.2.87 and its sub-lineage BA.2.87.1 was detected in South Africa, where 9 sequ ences of these were initially identified, there was a sort of a media blackout on emerging genomic SARS-CoV-2 sub-lineages and sequence uploads on GISAID have also dropped substantially! There was not much reports about further detection of BA.2.87 variants and its sub-lineages.
Certain doctors and researchers also have a hard time when they identify new SARS-CoV-2 variants circulating in certain countries as the health authorities and politicians in these countries do not like such news being disseminated as it thwarts their efforts in concealing the true COVID-19 situation in their countries as they want to project an image that everything is ok!
South African researchers involved with SARS-CoV-2 genomic surveillance after a recent tie up with an a Wellcome Sanger, a British research institute that is backed by the many big Pharmas, have also stopped revealing much about emerging variants and sub-lineages in South Africa!

 sangerinstitute.blog
sangerinstitute.blog
There are many anomalies that Thailand Medical News has been observing in the last 4 years with regards to identifying SARS-CoV-2 variants and sub-lineages and which sub-lineages are being chosen and monitored and the criteria for such selections etc plus the fact that all decisions to designate a sub-lineages are undertaken just by one young individual in based in an entity in Switzerland that is not directly or officially linked to the WHO and in which the young biostatistician involved has an active relationship with the WEF! Furthermore, while certain works are done on a collective basis with individuals coming various countries and walks or life, there is no proper organization, security vetting and background checks on the qualifications and backgrounds of some of these individuals. Some of their works begets questions for instance a certain Chinese scientist always simply focuses on identifying emerging variants only in India!
Another anomaly for instance is in Brazil especially in Mato Grosso. While Brazilian researchers identified the JN.2.5 sub-lineage as driving the surges there, there is no mention by these variant hunters involved with the Swiss entity or its platform Cov-Spectrum and neither is the JN.2.5 variant seen anywhere when current circulating variants for Brazil are searched on the CoV-Spectrum platform.
covSPECTRUM
Also, the labs in UK, Switzerland, Japan, USA and Germany doing studies on immune evasiveness, transmissibility and other properties of SARS-CoV-2 sub-lineages, completely ignored the JN.2.5 variant!
The same goes for other variants circulating in India such as the JN.1.11 and its spawns.
https://www.thailandmedical.news/ne...land-jn-2-5-causes-brazil-s-carnival-cancella
Thailand Medical News will be doing a separate expose on anomalies, in accuracies and possible bias in the identification of SARS-CoV-2 variants and sub-lineages in a collaboration with a few other media.
It should be noted that Dr Leshan Wannigamma has also been involved in the past with the promotion of Fluvoxamine to treat COVID-19!

 www.posttoday.com
www.posttoday.com
It was speculated that certain 'dubious' groups were behind this project to use fluvoxamine to treat COVID-19 such as groups linked to Zero COVID initiatives, the WHN and the NECSI including a Thai forest monkl from the North!
Hence, we recommend readers to be slightly skeptical till more details and proper validated evidence emerges about the detection of the BA.2.87.1 variants in South-East Asia.
Thailand Medical Authorities On Alert As Researcher Claims That New BA.2.87.1 Sub-Lineages Found In Wastewater Samples In South-East Asia
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 06, 2024
Thailand Medical authorities are on alert as a Sri Lankan researcher currently based in Japan has claimed that that the BA.2.87.1 sub-lineages have been detected in wastewater samples in South-East Asia. This is extremely interesting as this is the first time that there is any mention of the detection of the BA.2.87 or its sub-lineages BA.2.87.1 being detected out of South Africa since it was identified in early February 2024.
Dr Leshan Wannigama who had previously completed his PhD at the Chulalongkprn University in Thailand, and currently based in Yamagata Prefectural University of Health Sciences in Japan had posted online that the BA.2.87.1 sub-lineages had been found in waste water samples in South East Asia. He was also involved in waste water monitoring in Bangkok.
View: https://twitter.com/dr_leshan/status/1764186732701094143
He stopped short of identifying which South-East Asia countries in which these sub-lineages had been detected in and also he did not provide any further evidence of his claims but the rest of the ‘variant hunters’ online seem to have agreed with his claims.
Thailand Medical authorities, researchers and doctors have stepped up genomic surveillance in the country and hospitals are closely monitoring the situation. However, to date, there has been no official announcements that the BA.2.87.1 has been detected in the Thailand and it could possibility other South-East Asian countries that he was referring to.
A recent German research has been published as a preprint identifying the properties of this new BA.2.87.1 sub-lineages. Some of the unique properties of the BA.2.87.1 are worrying with implications of possible increased risk of disease severity upon being infected with such sub-lineages!

Virological traits of the SARS-CoV-2 BA.2.87.1 lineage
The highly mutated SARS-CoV-2 BA.2.87.1 lineage was recently detected in South Africa, but its transmissibility is unknown. Here, we report that BA.2.87.1 efficiently enters human cells but is more sensitive to antibody-mediated neutralization than the currently dominating JN.1 variant...
Interestingly the BA.2.87.1 sub-lineages were detected in waste water samples between December 2023 last week and January 2024 second week in South-East Asia according to Dr Wannigama.
View: https://twitter.com/dr_leshan/status/1764419784345575451
This raises a lot of questions as to whether the BA.2.87 variant originated in South Africa or elsewhere.
Interestingly after the BA.2.87 and its sub-lineage BA.2.87.1 was detected in South Africa, where 9 sequ ences of these were initially identified, there was a sort of a media blackout on emerging genomic SARS-CoV-2 sub-lineages and sequence uploads on GISAID have also dropped substantially! There was not much reports about further detection of BA.2.87 variants and its sub-lineages.
Certain doctors and researchers also have a hard time when they identify new SARS-CoV-2 variants circulating in certain countries as the health authorities and politicians in these countries do not like such news being disseminated as it thwarts their efforts in concealing the true COVID-19 situation in their countries as they want to project an image that everything is ok!
South African researchers involved with SARS-CoV-2 genomic surveillance after a recent tie up with an a Wellcome Sanger, a British research institute that is backed by the many big Pharmas, have also stopped revealing much about emerging variants and sub-lineages in South Africa!

Meet Professor Tulio de Oliveira, forging a genomic surveillance partnership - Wellcome Sanger Institute Blog
As head of the largest genomics institute in Africa and the Genomic Surveillance Unit’s new deputy director, Professor Tulio de Oliveira hopes close collaboration can be “world changing.”
There are many anomalies that Thailand Medical News has been observing in the last 4 years with regards to identifying SARS-CoV-2 variants and sub-lineages and which sub-lineages are being chosen and monitored and the criteria for such selections etc plus the fact that all decisions to designate a sub-lineages are undertaken just by one young individual in based in an entity in Switzerland that is not directly or officially linked to the WHO and in which the young biostatistician involved has an active relationship with the WEF! Furthermore, while certain works are done on a collective basis with individuals coming various countries and walks or life, there is no proper organization, security vetting and background checks on the qualifications and backgrounds of some of these individuals. Some of their works begets questions for instance a certain Chinese scientist always simply focuses on identifying emerging variants only in India!
Another anomaly for instance is in Brazil especially in Mato Grosso. While Brazilian researchers identified the JN.2.5 sub-lineage as driving the surges there, there is no mention by these variant hunters involved with the Swiss entity or its platform Cov-Spectrum and neither is the JN.2.5 variant seen anywhere when current circulating variants for Brazil are searched on the CoV-Spectrum platform.
covSPECTRUM
Also, the labs in UK, Switzerland, Japan, USA and Germany doing studies on immune evasiveness, transmissibility and other properties of SARS-CoV-2 sub-lineages, completely ignored the JN.2.5 variant!
The same goes for other variants circulating in India such as the JN.1.11 and its spawns.
https://www.thailandmedical.news/ne...land-jn-2-5-causes-brazil-s-carnival-cancella
Thailand Medical News will be doing a separate expose on anomalies, in accuracies and possible bias in the identification of SARS-CoV-2 variants and sub-lineages in a collaboration with a few other media.
It should be noted that Dr Leshan Wannigamma has also been involved in the past with the promotion of Fluvoxamine to treat COVID-19!

เปิดผลวิจัยเบื้องต้นกลุ่มยาทางเลือกรักษาโควิด ได้ผลดีกว่าฟาวิพิราเวียร์
กลุ่มวิจัยศึกษายาทางเลือกในการรักษาผู้ป่วยโควิดที่มีอาการไม่มากในไทย เผยผลเบื้องต้นได้ผลดีกว่าฟาวิพิราเวียร์ เดินหน้าทำการศึกษาเพิ่ม
It was speculated that certain 'dubious' groups were behind this project to use fluvoxamine to treat COVID-19 such as groups linked to Zero COVID initiatives, the WHN and the NECSI including a Thai forest monkl from the North!
Hence, we recommend readers to be slightly skeptical till more details and proper validated evidence emerges about the detection of the BA.2.87.1 variants in South-East Asia.
Heliobas Disciple
TB Fanatic

Here's more on this:

Scientists may have finally found the cause of long Covid
Scientists at Cambridge University believe low iron levels in the blood - and the body's ability to regulate this important nutrient - could be a key driver of ongoing issues with long Covid.
Scientists may have finally found the cause of long Covid: Low iron levels after infection 'might be trigger of poorly-understood illness'
By Xantha Leatham, Deputy Science Editor For The Daily Mail
Published: 09:51 EST, 4 March 2024 | Updated: 12:03 EST, 4 March 2024
- 1.9 million people in the UK alone say they experience symptoms of long Covid
- Scientists found those with long Covid had problems with iron levels in blood
Experts may have found the cause of long Covid after discovering that low iron levels following an infection could be a key trigger.
An estimated 1.9 million people in the UK alone say they experience symptoms of long Covid.
These can include fatigue, shortness of breath, muscle aches and problems with memory and concentration – and last long after the initial Covid infection has subsided.
Now scientists believe that problems with iron levels in the blood – and the body’s ability to regulate this important nutrient – could be a key driver of ongoing issues.
And the discovery could point to possible ways to prevent or treat the condition.
Shortly after the start of the pandemic, a team led by Cambridge University began recruiting people who had tested positive for the virus.
Over the course of a year, participants provided blood samples and it became clear that a significant number of patients would go on to have symptoms that persisted.
In the end the researchers focused their analysis on 214 individuals, around half of whom reported long Covid symptoms between three and 10 months after their infection.
They discovered that ongoing inflammation and low iron levels in the blood could be seen as early as two weeks following an infection in those individuals reporting long Covid many months later.
Problems with iron levels in the blood were detectable in the long Covid group regardless of age, sex or infection severity, they found.
Dr Aimee Hanson, who worked on the study while at the University of Cambridge and is now at the University of Bristol, said: ‘Iron levels, and the way the body regulates iron, were disrupted early on during SARS-CoV-2 infection, and took a very long time to recover, particularly in those people who went on to report long Covid months later.
‘Although we saw evidence that the body was trying to rectify low iron availability and the resulting anaemia by producing more red blood cells, it was not doing a particularly good job of it in the face of ongoing inflammation.’
Co-author Professor Hal Drakesmith, from the University of Oxford, said iron dysregulation is a natural response to infection.
‘When the body has an infection, it responds by removing iron from the bloodstream,’ he said.
‘This protects us from potentially lethal bacteria that capture the iron in the bloodstream and grow rapidly. It’s an evolutionary response that redistributes iron in the body, and the blood plasma becomes an iron desert.
‘However, if this goes on for a long time, there is less iron for red blood cells, so oxygen is transported less efficiently affecting metabolism and energy production, and for white blood cells, which need iron to work properly. The protective mechanism ends up becoming a problem.’
The findings, published in the journal Nature Immunology, may help explain why symptoms such as fatigue and exercise intolerance are common in long Covid.
The researchers say the study points to potential ways of preventing or reducing the impact of long Covid by rectifying iron dysregulation during early infection.
One approach might be controlling the extreme inflammation as early as possible, before it impacts on iron regulation.
Another approach might involve iron supplementation - however as Dr Hanson pointed out, this may not be straightforward.
‘It isn't necessarily the case that individuals don't have enough iron in their body, it's just that it’s trapped in the wrong place,’ she said.
‘What we need is a way to remobilise the iron and pull it back into the bloodstream, where it becomes more useful to the red blood cells.’
Heliobas Disciple
TB Fanatic

9 New ‘Independent’ Advisers to CDC Publicly Promoted Vaccines or Took Money From Pharma — or Both
After struggling for months to fill seats on the Centers for Disease Control and Prevention’s vaccine advisory committee, the U.S. Department of Health and Human Services announced nine new appointees. All have financial ties to vaccine makers or have publicly promoted COVID-19, RSV and HPV...
9 New ‘Independent’ Advisers to CDC Publicly Promoted Vaccines or Took Money From Pharma — or Both
After struggling for months to fill seats on the Centers for Disease Control and Prevention’s vaccine advisory committee, the U.S. Department of Health and Human Services announced nine new appointees. All have financial ties to vaccine makers or have publicly promoted COVID-19, RSV and HPV vaccines — or both.
Brenda Baletti, Ph.D.
03/06/24
Nine new members named to the committee that advises the Centers for Disease Control and Prevention (CDC) on vaccine recommendations have financial ties to pharmaceutical companies or have worked with public health agencies to promote the COVID-19, RSV or HPV vaccines.
The U.S. Department of Health and Human Services (HHS) in mid-February appointed the new members to the Advisory Committee on Immunization Practices (ACIP), which shapes U.S. vaccine policy.
Commenting on the new appointments, Children’s Health Defense (CHD) President Mary Holland said:
“ACIP has long been a rubber stamp for any and all vaccines Big Pharma wants to push. But the brazenness of the HHS-Big Pharma fusion has never been so much on display.
“The only silver lining in this grotesque display is that more and more people are waking up to the reality that ACIP has nothing to do with health and everything to do with profit.”
The ACIP is described as an independent, nonfederal expert body made up of professionals with clinical, scientific and public health expertise. The committee decides which vaccines should be recommended to the public, who should take them and how often — recommendations the CDC typically rubber stamps.
This external advisory committee includes a chair, an executive secretary, and 15 voting members — 14 medical experts and a lay member representing consumers.
It also includes a non-voting body that offers input composed of eight ex officio members from other federal health departments and liaison representatives from health-related professional organizations like the American Association of Pediatrics.
However, when the committee convened last week to make its spring recommendations, it was missing so many voting members that it lacked a quorum. Vacant committee spaces on the “independent” committee had to be temporarily filled by government employees — ex officio members can be sworn in as temporary voting members.
Over the last year, HHS struggled to fill eight vacancies. An additional four members will be needed when existing members’ four-year terms are up at the end of June.
As seats on the committee sat unfilled, industry news sites like StatNews suggested the committee “appears to be atrophying” and Medriva said there is an “unprecedented lack of expertise in the committee.”
When HHS finally announced the new members to fill the vacancies, it was also reported the new members would be filling spots at last week’s meeting. However, they had not yet taken their positions at the time the meeting occurred on Feb. 28-29.
A CDC spokesperson confirmed to The Defender that nine members have been appointed to the committee, including Dr. Helen Keipp Talbot, an infectious diseases researcher at Vanderbilt University who previously served on the committee from 2018 through 2022 and will rejoin the committee to serve as chair.
Members typically are not eligible for reappointment, but in Talbot’s case, the HHS provided a waiver to that existing policy.
In addition to Talbot, four members will begin their tenure immediately upon submission of paperwork. These include Dr. Denise Jamieson, dean of the University of Iowa Carver College of Medicine; Dr. Yvonne Maldonado, a professor of pediatrics at Stanford University; Dr. Robert Schechter, a medical officer with the California Department of Public Health; and Dr. Albert Shaw, an infectious diseases professor at the Yale School of Medicine.
The other appointees will begin on July 1. They include Dr. Edwin Asturias, a pediatric infectious diseases specialist at the Colorado School of Public Health; Noel Brewer, Ph.D., a professor of health behavior at the University of North Carolina; Dr. Helen Chu, an infectious diseases specialist at the University of Washington; and Dr. George Kuchel, a professor of geriatric medicine at the University of Connecticut.
All nine appointees will serve four-year terms.
“Stringent measures and rigorous screening” are reportedly used to avoid the committee members having “real or apparent” conflicts of interest.
However, all of the new appointees except for the public member have received grant funding or consulting fees from major pharmaceutical companies, including vaccine makers like Pfizer, Moderna and Merck, or have worked for HHS or on recent HHS grants developing or testing vaccines or investigating how to improve vaccine uptake.
Many of them have been key public advocates for the COVID-19, respiratory syncytial virus (RSV) and human papillomavirus (HPV) vaccines, crafting and promoting the CDC’s message in the media and in the clinic.
Several have sat, sometimes together, on other vaccine advisory committees for the World Health Organization (WHO), the state of California, and The Lancet, among others.
What constitutes a conflict of interest?
The committee’s policies and procedures document, updated in 2022, defines a “conflict of interest” for committee members.
According to the ACIP policies, while members are actively on the committee, neither they nor their immediate families can be employed by or hold stock in a vaccine manufacturer. They cannot receive royalties from a vaccine that is being evaluated by the committee. They cannot act as advisers, consultants or a paid litigation expert to a vaccine manufacturer, or otherwise receive money from a vaccine maker — with exceptions — while they serve on the committee.
The committee’s definition of a conflict of interest doesn’t prohibit members from benefiting financially from HHS grants while on the committee.
It also doesn’t apply to their activities before or after their time on the committee, which is when most potential members have taken money from industry or engaged in vaccine promotion that raises questions about their impartiality.
This narrowly defined conflict of interest differs markedly from how HHS defines conflict of interest in its ethics training for HHS employees. In that training, HHS warns employers that criminal law prohibits them “from participating personally or substantially in an official capacity that would have a direct and predictable defect on your financial interests,” according to a source at the CDC who asked not to be named.
HHS also notes in its training that “appearances matter” and a conflict of interest arises if a reasonable person with knowledge of relevant facts would question someone’s impartiality.
Impartiality is not a requirement for membership on the CDC advisory committee. Members are required only to declare their financial conflicts at each meeting and to recuse themselves where appropriate.
Members may be granted waivers if the committee’s need for their services outweighs the conflict of interest, according to the CDC.
Below are the new appointees, with a summary of their research and their links to Pharma or public health agencies and research that could raise questions about their impartiality.
Jamieson promoted COVID vaccines for pregnant women
Dr. Denise Jamieson spent most of her career working for the CDC before becoming a faculty member at Emory University and then a dean at the University of Iowa.
Jamieson is a spokesperson for the American College of Obstetricians and Gynecologists and a member of its Practice Advisory on COVID-19 Vaccines and Pregnancy.
She publicly promoted the COVID-19 vaccine as “safe and effective” for pregnant women as early as Spring 2021 — even though in January 2021, regulatory agencies were aware from Pfizer’s own data that the vaccines pose serious risks for pregnant women.
The American College of Obstetricians and Gynecologists recommended pregnant women get vaccinated despite a lack of clinical trials showing safety and even before the CDC began advising pregnant women to take the vaccine.
The association was among the many women’s health organizations that had urged Pfizer and Moderna to speed up vaccine tests in pregnant women, The New York Times reported.
Last year, Freedom of Information Act requests revealed the CDC bankrolled the association to the tune of $11 million to promote COVID-19 vaccination as “safe and effective” for pregnant women.
As part of her public outreach promoting the COVID-19 vaccines, Jamieson said in public interviews that fertility concerns about the vaccines were “myths” with “no biological plausibility.
Jamieson also said there was no evidence that the vaccines caused menstrual irregularities, despite early reports that vaccines were causing menstrual irregularities. She also began advocating vaccination for adolescent girls even before the vaccines were approved for adolescents.
Maldonado studied COVID vaccines in children for Pfizer
Stanford’s Dr. Yvonne Maldonado took tens of thousands of dollars in consulting fees and nearly $4 million in research funding from Pfizer since 2016, according to OpenPaymentsData.CMS.gov, the government website that tracks pharmaceutical industry funding to medical professionals.
She also received consulting fees for Trumenba, a meningococcal vaccine for meningitis B.
Among the projects she has headed up are studies of nasal swab techniques that led to home testing and the development of an antibody test to detect the virus, which received U.S. Food and Drug Administration (FDA) approval.
Maldonado was a strong public advocate for testing the vaccines in children. She promoted testing the vaccines on kids in outlets like NBC News as early as October 2020, despite acknowledging children were at very low risk for serious illness.
She led clinical trials for the Pfizer-BioNTech COVID-19 vaccine in children at Stanford, promoted them as 90% effective for children and was an early advocate for including the vaccines on the childhood immunization schedule.
In this video from November 2021, Maldonado celebrates the short amount of time it took to make the vaccines and promotes them for children:
3 min 19 sec
Maldonado also advocated to expand the use of Paxlovid for children.
The Bill & Melinda Gates Foundation recently funded the Maldonado Group to do a 2.5-year study on the oral poliovirus vaccine in Veracruz, Mexico.
Experts have widely criticized the Gates Foundation for over a decade for its self-interested work promoting polio vaccines in the developing world at the expense of other, more important public health measures.
Shaw, a strong COVID vaccine advocates
Albert Shaw, M.D., Ph.D., studies the immunology of aging at the Yale School of Medicine. He recently was the principal investigator on a major observational study of adults hospitalized with COVID-19, funded by the National Institute of Allergy and Infectious Diseases.
Shaw also publicly advocated for COVID-19 vaccination, particularly for the elderly and for pregnant mothers. He appears frequently on local news sounding the alarm on the dangers of COVID-19, even for strains like XBB 1.5, promoting the vaccines as “safe and effective” and encouraging people to get vaccinated and boosted.
OpenPaymentsData reports that Shaw was paid $2,590.00 in consulting fees by Boehringer Ingelheim Pharmaceuticals Inc. in 2022 and $1,425.71 from GSK (formerly GlaxoSmithKline) in 2019.
Schechter, a ‘public advocate’ on multiple HHS committees
Dr. Robert Schechter appears to hold the position of the public member, meant to represent consumers on the committee. Schechter also serves as the public member of the National Vaccine Advisory Committee, another HHS vaccine advisory committee.
However, he was a medical officer with the California Department of Public Health for decades working primarily on the California Vaccines for Children Program.
He has functioned as a spokesperson, informing the public about vaccines in California, frequently quoted in local media. He also is a member of the American Association of Pediatrics.
Schechter also served on the California Department of Public Health Western States Scientific Safety Review Workgroup, along with other existing and incoming members of the CDC advisory committee Maldonado and former chair Dr. Grace Lee. That group set COVID-19 vaccine and booster recommendations.
Asturias, a global vaccine researcher with consulting fees from 5 Pharma companies
Dr. Edwin Asturias is a professor of pediatrics with a focus on Latin America. He has served on several different vaccine advisory boards globally, including in Guatemala and for the WHO.
Asturias is a member of the Strep A Vaccine Global Consortium whose mission is to make sure Strep A vaccines are available and administered. He also receives grant funding from Pfizer and is a paid consultant for Curevac, Inovio and Moderna.
Much of his research focuses on the epidemiology of disease, largely in rural Guatemala. However, over the last several years Asturias has published several articles on “vaccine hesitancy” among rural Latin American people and how to overcome it.
He has worked on several studies of community perceptions of vaccines in his native Guatemala, including studies of attitudes among trusted leaders and parents who are key to building vaccine confidence.
According to OpenPaymentsData, Asturias received approximately $4,000 in consulting fees and over $1 million in research funding from Merck in 2022.
Since 2016, Asturias has received over $60,000 in consulting fees and travel costs from Merck, Pfizer, GSK, Sanofi Pasteur and Astellas Pharma, and almost $3 million in research funding from Pfizer, over $750,000 in research funding from GSK and a small amount of funding from Takeda Vaccines.
That is in addition to tens of thousands of dollars in payments from those same companies in 2014.
[continued next post]
Heliobas Disciple
TB Fanatic
[continued from above post]
Brewer, a Merck consultant who developed the ‘Announcement Approach’ to HPV vaccination
Asturias will be joined on the committee by another Merck consultant and “vaccine hesitancy” expert, Noel Brewer, Ph.D.
Brewer is a behavioral psychologist at the University of North Carolina’s Gillings School of Public Health, a paid consultant for Merck and the recipient of commercial research grants from Merck, Pfizer and GSK.
Over the past several years, Brewer received millions of dollars in funding from HHS for research on how to increase teen uptake of the HPV vaccine, documents obtained by CHD via a Freedom of Information Act request revealed.
Merck, for which Brewer consults, makes Gardasil, the only HPV vaccine commercially available in the U.S.
Brewer is best known for developing and testing the “Announcement Approach” to vaccinating the vaccine-hesitant. The approach involves having providers skip the step of discussing with families in “open-ended conversation” whether or not they want their child vaccinated for HPV and instead “presume” the family wants the vaccine and announce the child will receive it as if it were a routine part of the office visit.
Brewer and others’ previous research shows this method reduces the time a provider needs to spend talking with their patients and increases vaccine uptake.
HHS also has dedicated millions of dollars in funding to other researchers to test ways to expand Brewer’s approach.
In what was perhaps a Freudian slip, Brewer announced his new appointment on X, formerly Twitter, saying the committee would be setting the “vaccine police”:
Chu has ties to Pharma, Gates ventures and is an advocate for the RSV vaccine
Dr. Helen Chu is an infectious disease specialist and co-author of the JAMA study that concluded the COVID-19 bivalent boosters were effective in children and adolescents ages 5-17.
Chu has consulted for pharmaceutical companies AbbVie, Vindico, Ellume, Medscape, Merck, Clinical Care Options, Catalyst Medical Education, Vir, Pfizer, Prime Education and the Gates Foundation.
She also served on advisory boards for Vir, Merck and AbbVie and conducted continuing medical education teaching with Medscape, Vindico, Catalyst CME and Clinical Care Options.
Gates Ventures has published her research and she also obtained support from Cepheid, a PCR testing company.
As an RSV researcher, Chu early on, on X (formerly Twitter), raised the alarm about a “triple-demic” dangerous for children and the elderly.
Later, she promoted the RSV vaccine, particularly for pregnant women. She is a co-author of a systematic review in The Lancet, out this month, finding that infants, particularly pre-term babies, have a higher risk for RSV-related severe acute lower respiratory infection.
Chu and her co-authors conclude: “Preventive products for RSV can have a substantial public health impact by preventing RSV-associated … severe outcomes from infection in preterm infants,“ a finding that implies vaccination during pregnancy or of infants would be appropriate, as these are the measures currently available or being considered.
GSK halted its Phase 3 clinical trial of RSV in pregnant women in 2022 after the company identified a safety signal for preterm birth. Pfizer was criticized for not informing women of the risk, the BMJ reported. Pfizer’s version of the RSV vaccine received FDA approval after Chu presented her research to the FDA’s vaccine advisory committee in May.
After the FDA approved it, the CDC advisory committee that Chu will sit on recommended it.
In less than a year since its approval, CDC data and the Vaccine Adverse Event Reporting System (VAERS) already show reports of 34 deaths, 302 serious adverse events and according to news reports this week, a safety signal for Guillain-Barré syndrome, The Defender reported.
As an example of her Pharma-funded educational work, in March, Chu presented a Pfizer-funded webinar to educate providers on “the burden of RSV in older adults” and the “importance of RSV awareness.”
Kuchel strongly advocates the RSV vaccine for pregnant women and the elderly
Dr. George Kuchel, professor of geriatric medicine is a strong advocate for the RSV vaccine in pregnant women and older people. He promoted the vaccine as potentially “transformational” for older people — just like the COVID-19 and flu vaccines, he said.
In 2023, Kuchel told the media there was no evidence the vaccine posed a risk to pregnant women, despite the safety signals in GSK’s trials.
Kuchel is currently working on a five-year, $9 million grant from the National Institute of Allergy and Infectious Diseases to study flu vaccines in older adults.
According to OpenPaymentsData, he has taken consulting fees — approximately $13,000 from Janssen Global Service in 2019 and approximately $1,300 from Novo Nordisk in 2020.
Former member Talbot replaces Lee as chair
The final new appointee, former committee member Dr. Helen Keipp Talbot, will rejoin the committee as chair. Her research focuses on adult vaccination, influenza vaccination, human coronaviruses and vaccine trials for respiratory illnesses such as RSV.
According to Talbot’s curriculum vitae — last updated in 2018 before she joined the committee — her most recent research funding comes from both the federal government (CDC, National Institutes of Health) and Sanofi Pasteur, primarily for the study of pandemic preparedness in 2015 and influenza vaccination.
Sanofi and MedImmune have been recurrent funders since 2009, along with AstraZeneca, Gilead, Protein Sciences, VaxInnate and Wyeth (since acquired by Pfizer).
According to the OpenPaymentsData, Talbot received roughly $1.4 million in research payments and associated research funding since 2014 (417 total payments) from these companies, along with 29 general payments totaling $17,000, The Defender reported.
Talbot sat on the committee through the pandemic that voted to recommend the COVID-19 vaccines and boosters for adults and children.
Talbot will replace former chair, Dr. Grace Lee, who was associate chief medical officer for practice innovation at Stanford Medicine Children’s Health and a pediatrics professor at Stanford School of Medicine since 2017.
While committee appointments are typically four years long, Lee served only two, and the chair position currently sits vacant. Her office did not respond to The Defender’s inquiry as to why she resigned from the committee.
While she was on the committee, her husband, Joshua Salomon, Ph.D., health policy professor at Stanford was heading up a major, multi-million dollar five-year CDC-funded project to model local and national policies for responding to infectious diseases. That work is also funded by the Gates Foundation.
Brewer, a Merck consultant who developed the ‘Announcement Approach’ to HPV vaccination
Asturias will be joined on the committee by another Merck consultant and “vaccine hesitancy” expert, Noel Brewer, Ph.D.
Brewer is a behavioral psychologist at the University of North Carolina’s Gillings School of Public Health, a paid consultant for Merck and the recipient of commercial research grants from Merck, Pfizer and GSK.
Over the past several years, Brewer received millions of dollars in funding from HHS for research on how to increase teen uptake of the HPV vaccine, documents obtained by CHD via a Freedom of Information Act request revealed.
Merck, for which Brewer consults, makes Gardasil, the only HPV vaccine commercially available in the U.S.
Brewer is best known for developing and testing the “Announcement Approach” to vaccinating the vaccine-hesitant. The approach involves having providers skip the step of discussing with families in “open-ended conversation” whether or not they want their child vaccinated for HPV and instead “presume” the family wants the vaccine and announce the child will receive it as if it were a routine part of the office visit.
Brewer and others’ previous research shows this method reduces the time a provider needs to spend talking with their patients and increases vaccine uptake.
HHS also has dedicated millions of dollars in funding to other researchers to test ways to expand Brewer’s approach.
In what was perhaps a Freudian slip, Brewer announced his new appointment on X, formerly Twitter, saying the committee would be setting the “vaccine police”:
Excited to announce that I’ve been appointed as a voting member of ACIP, the CDC board that sets vaccine police for the US. HHS fills key vaccine advisory panel slots
— Noel Brewer (@noelTbrewer) February 16, 2024
Dr. Peter Hotez responded with his congratulations. The two worked together on the Lancet Commission of Vaccine Refusal, Acceptance and Demand in the USA, which was “formed to address the persistent and important threat to public health in the USA posed by suboptimal uptake of some vaccines.”Chu has ties to Pharma, Gates ventures and is an advocate for the RSV vaccine
Dr. Helen Chu is an infectious disease specialist and co-author of the JAMA study that concluded the COVID-19 bivalent boosters were effective in children and adolescents ages 5-17.
Chu has consulted for pharmaceutical companies AbbVie, Vindico, Ellume, Medscape, Merck, Clinical Care Options, Catalyst Medical Education, Vir, Pfizer, Prime Education and the Gates Foundation.
She also served on advisory boards for Vir, Merck and AbbVie and conducted continuing medical education teaching with Medscape, Vindico, Catalyst CME and Clinical Care Options.
Gates Ventures has published her research and she also obtained support from Cepheid, a PCR testing company.
As an RSV researcher, Chu early on, on X (formerly Twitter), raised the alarm about a “triple-demic” dangerous for children and the elderly.
Later, she promoted the RSV vaccine, particularly for pregnant women. She is a co-author of a systematic review in The Lancet, out this month, finding that infants, particularly pre-term babies, have a higher risk for RSV-related severe acute lower respiratory infection.
Chu and her co-authors conclude: “Preventive products for RSV can have a substantial public health impact by preventing RSV-associated … severe outcomes from infection in preterm infants,“ a finding that implies vaccination during pregnancy or of infants would be appropriate, as these are the measures currently available or being considered.
GSK halted its Phase 3 clinical trial of RSV in pregnant women in 2022 after the company identified a safety signal for preterm birth. Pfizer was criticized for not informing women of the risk, the BMJ reported. Pfizer’s version of the RSV vaccine received FDA approval after Chu presented her research to the FDA’s vaccine advisory committee in May.
After the FDA approved it, the CDC advisory committee that Chu will sit on recommended it.
In less than a year since its approval, CDC data and the Vaccine Adverse Event Reporting System (VAERS) already show reports of 34 deaths, 302 serious adverse events and according to news reports this week, a safety signal for Guillain-Barré syndrome, The Defender reported.
As an example of her Pharma-funded educational work, in March, Chu presented a Pfizer-funded webinar to educate providers on “the burden of RSV in older adults” and the “importance of RSV awareness.”
Kuchel strongly advocates the RSV vaccine for pregnant women and the elderly
Dr. George Kuchel, professor of geriatric medicine is a strong advocate for the RSV vaccine in pregnant women and older people. He promoted the vaccine as potentially “transformational” for older people — just like the COVID-19 and flu vaccines, he said.
In 2023, Kuchel told the media there was no evidence the vaccine posed a risk to pregnant women, despite the safety signals in GSK’s trials.
Kuchel is currently working on a five-year, $9 million grant from the National Institute of Allergy and Infectious Diseases to study flu vaccines in older adults.
According to OpenPaymentsData, he has taken consulting fees — approximately $13,000 from Janssen Global Service in 2019 and approximately $1,300 from Novo Nordisk in 2020.
Former member Talbot replaces Lee as chair
The final new appointee, former committee member Dr. Helen Keipp Talbot, will rejoin the committee as chair. Her research focuses on adult vaccination, influenza vaccination, human coronaviruses and vaccine trials for respiratory illnesses such as RSV.
According to Talbot’s curriculum vitae — last updated in 2018 before she joined the committee — her most recent research funding comes from both the federal government (CDC, National Institutes of Health) and Sanofi Pasteur, primarily for the study of pandemic preparedness in 2015 and influenza vaccination.
Sanofi and MedImmune have been recurrent funders since 2009, along with AstraZeneca, Gilead, Protein Sciences, VaxInnate and Wyeth (since acquired by Pfizer).
According to the OpenPaymentsData, Talbot received roughly $1.4 million in research payments and associated research funding since 2014 (417 total payments) from these companies, along with 29 general payments totaling $17,000, The Defender reported.
Talbot sat on the committee through the pandemic that voted to recommend the COVID-19 vaccines and boosters for adults and children.
Talbot will replace former chair, Dr. Grace Lee, who was associate chief medical officer for practice innovation at Stanford Medicine Children’s Health and a pediatrics professor at Stanford School of Medicine since 2017.
While committee appointments are typically four years long, Lee served only two, and the chair position currently sits vacant. Her office did not respond to The Defender’s inquiry as to why she resigned from the committee.
While she was on the committee, her husband, Joshua Salomon, Ph.D., health policy professor at Stanford was heading up a major, multi-million dollar five-year CDC-funded project to model local and national policies for responding to infectious diseases. That work is also funded by the Gates Foundation.
Heliobas Disciple
TB Fanatic
New Study Finds That Persistent COVID-19 Infections Are Surprisingly Common
Recent research conducted by the University of Oxford has found that a high proportion of SARS-CoV-2 infections in the general population lead to persistent infections lasting a month or more. The findings have been published in the journal Nature. It has long been thought that prolonged COVID-19
scitechdaily.com
New Study Finds That Persistent COVID-19 Infections Are Surprisingly Common
By University of Oxford
March 5, 2024
Recent research conducted by the University of Oxford has found that a high proportion of SARS-CoV-2 infections in the general population lead to persistent infections lasting a month or more. The findings have been published in the journal Nature.
It has long been thought that prolonged COVID-19 infections in immunocompromised individuals may have been the source of the multiple new variants that arose during the coronavirus pandemic and seeded successive waves of infection, including the Alpha and Omicron variants. But until now, the prevalence of persistent COVID-19 infections in the general population and how the virus evolves in these situations remained unknown.
Study Methodology and Findings
To investigate this, the researchers used data from the Office for National Statistics Covid Infection Survey (ONS-CIS), which tested participants approximately monthly. Of the 90,000+ participants, 3,603 provided two or more positive samples between November 2020 to August 2022 where the virus was sequenced. Of these, 381 individuals tested positive for the same viral infection over a period of a month or longer. Within this group, 54 individuals had a persistent infection that lasted at least two months. The researchers estimate that between one in a thousand to one in 200 (0.1-0.5%) of all infections may become persistent, and last for at least 60 days.
In some cases, individuals remained infected with viral variants that had gone extinct in the general population. In contrast, the researchers found that reinfection with the same variant was very rare, likely due to the host developing immunity to that variant and the variant reducing in frequency to very low levels after a few months.
Insights into Viral Dynamics and Long-COVID
Of the 381 persistent infections, 65 had three or more PCR tests taken over the course of their infection. Most (82%) of these individuals demonstrated rebounding viral dynamics, experiencing high, then low, then high viral load dynamics. According to the researchers, this demonstrates that the virus can maintain the ability to actively replicate during prolonged infections.
In the study, people with persistent infections were 55% more likely to report having Long COVID symptoms more than 12 weeks since the start of the infection than people with more typical infections.
Certain individuals showed an extremely high number of mutations, including mutations that define new coronavirus variants, alter target sites for monoclonal antibodies, and introduce changes to the coronavirus spike protein. However, most individuals did not harbor a large number of mutations, suggesting that not every persistent infection will be a potential source for new concerning variants.
Co-lead author of the study Dr Mahan Ghafari (Pandemic Sciences Institute, Nuffield Department of Medicine, University of Oxford) said: ‘Our observations highlight the continuing importance of community-based genomic surveillance both to monitor the emergence and spread of new variants, but also to gain a fundamental understanding of the natural history and evolution of novel pathogens and their clinical implications for patients.’
Co-lead author Dr Katrina Lythgoe (Department of Biology and Pandemic Sciences Institute, University of Oxford) said: ‘Although the link between viral persistence and Long Covid may not be causal, these results suggest persistent infections could be contributing to the pathophysiology of Long Covid. Indeed, many other possible mechanisms have been suggested to contribute to Long Covid including inflammation, organ damage, and microthrombosis.’
Reference: “Prevalence of persistent SARS-CoV-2 in a large community surveillance study” by Mahan Ghafari, Matthew Hall, Tanya Golubchik, Daniel Ayoubkhani, Thomas House, George MacIntyre-Cockett, Helen R. Fryer, Laura Thomson, Anel Nurtay, Steven A. Kemp, Luca Ferretti, David Buck, Angie Green, Amy Trebes, Paolo Piazza, Lorne J. Lonie, Ruth Studley, Emma Rourke, Darren L. Smith, Matthew Bashton, Andrew Nelson, Matthew Crown, Clare McCann, Gregory R. Young, Rui Andre Nunes dos Santos, Zack Richards, Mohammad Adnan Tariq, Roberto Cahuantzi, Wellcome Sanger Institute COVID-19 Surveillance Team, COVID-19 Infection Survey Group, The COVID-19 Genomics UK (COG-UK) Consortium, Jeff Barrett, Christophe Fraser, David Bonsall, Ann Sarah Walker and Katrina Lythgoe, 21 February 2024, Nature.
DOI: 10.1038/s41586-024-07029-4
Last edited:
Heliobas Disciple
TB Fanatic

Model estimates who benefits most from frequent COVID-19 boosters
Patients kept asking a question that Nathan Lo, MD, Ph.D., infectious disease specialist, had a hard time answering: How often should I get my booster shot for COVID-19?
Model estimates who benefits most from frequent COVID-19 boosters
by Stanford University Medical Center
March 6, 2024
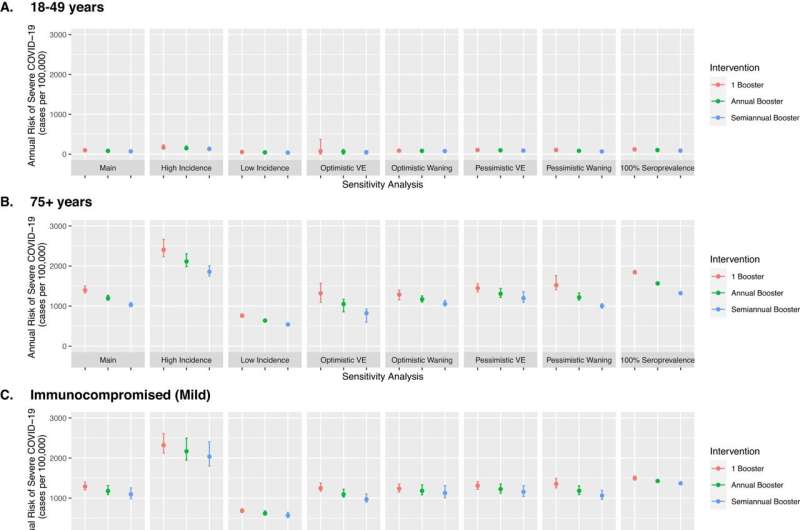
Sensitivity analysis of model parameters for COVID-19 risk and booster vaccination. We plotted results for three representative risk groups: 18–49 years (A), 75+ years (B), and the mild immunocompromised population (C). Credit: Nature Communications (2024). DOI: 10.1038/s41467-024-45549-9
Patients kept asking a question that Nathan Lo, MD, Ph.D., infectious disease specialist, had a hard time answering: How often should I get my booster shot for COVID-19?
"It's a question that we have all asked. My patients have asked; friends and family members have asked," Lo said. "We point to the national vaccine recommendations, although increasingly this question has become challenging to answer. I didn't quite have the estimates on hand that I might hope to share with patients."
To build that evidence, Lo and his team at Stanford Medicine turned to their area of expertise, computational modeling. The researchers developed a simulation model using Centers for Disease Control and Prevention COVID-19 surveillance data and vaccine effectiveness estimates to predict the frequency of COVID-19 vaccination that best prevents severe disease in different U.S. populations.
They published a study describing that model and its results in the journal Nature Communications, led by Lo, who is the senior author of the study and an assistant professor of medicine.
The model's results largely square with data on who is most at risk of bad outcomes from COVID-19: For those older than 65 or who are immunocompromised, more frequent boosters—at least annually—go further to protect against hospitalization or death. For younger populations, the benefit of frequent boosting against severe disease is more modest.
The researchers hope this model can help inform both individuals making decisions about when to get boosters as well as public health policy makers.
"We're in the fourth year of the pandemic now, and we're shifting toward more long-term mitigation strategies," said Stanford Medicine research data scientist Hailey Park, who is the lead author on the study. "We know that protection from vaccination wanes, and we know that disease risk is very heterogeneous in the population. So how do we come up with a more optimal timing for boosters?"
Simulating the population
The model is what's known as a microsimulation, meaning it simulates a large population with results at the individual level, Park said. She and her colleagues built a simulation of millions of individuals with their unique traits, aiming to mimic the overall U.S. adult population—except these simulated people had received their initial COVID-19 vaccinations.
Using the CDC's weekly COVID-19 surveillance data starting in September 2022, when the bivalent booster was first available, the model predicted how many severe infections leading to hospitalization or death would result in different age or health status groups over the course of two years. The team estimated outcomes if those individuals received just one COVID booster, a booster every year or a shot every six months.
For those over 75 years, receiving a yearly booster reduced annual severe infections from around 1,400 cases per 100,000 people to about 1,200 cases. Bumping the booster up to twice a year dropped severe infections to just over 1,000 per 100,000.
The numbers are similar for those who are moderately or severely immunocompromised, and about half that reduction for those aged 65 to 74. For younger, healthy people, the drop is much smaller: Annual or twice-yearly boosters reduced severe infections in people aged 18 to 49 by only 14 to 26 cases per 100,000 people.
"These high-risk populations benefit from more frequent boosters relative to younger and healthier individuals, and I think that's intuitive," Lo said. "But it's helpful to see the numbers; what is the difference in magnitude of risk?"
These findings support current CDC recommendations and the benefit of at least annual boosters to people 65 and older and immunocompromised populations, and suggest that public health strategies to increase booster uptake could get the most bang for their buck by focusing on the high-risk populations.
A thorny question
"In this study we focused on a goal of reducing severe COVID-19 leading to hospitalization, but there are numerous other considerations that influence vaccine decisions," Lo said.
The team considered how novel variants and overall transmission play into decisions on how frequently to receive booster vaccines. They looked at the effect of new viral variants with regard to evasion of the immune system and found that the benefit of more frequent boosters for all groups was larger if new vaccine formulations were better matched to the latest variants.
In addition, the team looked at the impact of transmission: Compared with more restricted booster programs targeting only higher risk populations, more inclusive frequent booster programs (for all age and risk groups) led to lower transmission, with additional benefit for the highest risk groups.
The researchers note that frequent vaccination also helped reduce non-severe cases in all risk groups. "There are a multitude of considerations here, and the optimal vaccine recommendations will depend on what is factored into the decision," Lo said.
The scientists also included prior COVID-19 infection in their model, finding less benefit from frequent vaccination to prevent severe disease for those who had previously had a case of COVID-19 compared with those who hadn't. Prior infection gives a short window of protection against infection, so the booster's protection on top of that is smaller.
Due to a lack of data and to simplify the model, some variables weren't accounted for in the study: The likelihood of infection for each group was assumed to be the same over time, even though infection risk differs in real life.
The model was also based on data from earlier circulating variants and vaccine formulations. Immunocompromised people were clustered into two groups in the model, although these populations are actually much more variable, and the model did not address vaccine hesitancy or the risks of long COVID.
Lo and his colleagues plan to share their findings with policymakers and will update the model with new data as it becomes available, hoping to shed even more light on the tricky question of vaccine frequency.
"In science, there are some questions that get easier over time and some that get more challenging over time," Lo said. "This is one of the latter."
Researchers from the Yale School of Public Health; the University of California, San Francisco; and the California Department of Public Health also contributed to the study.
More information: Hailey J. Park et al, Comparing frequency of booster vaccination to prevent severe COVID-19 by risk group in the United States, Nature Communications (2024). DOI: 10.1038/s41467-024-45549-9
Provided by Stanford University Medical Center
Heliobas Disciple
TB Fanatic
(fair use applies)
Parana, A State In Brazil Currently Inundated With Rising COVID-19 Infections. JN.2.5 And JN.1.7 Variants Possibly At Play
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 07, 2024
The state of Paraná in Brazil finds itself once again grappling with a surge in COVID-19 infections, driven by the emergence of the JN.2.5 and JN.1.7 variants. The Municipal Health Department is sounding the alarm as the number of daily cases has skyrocketed, posing a significant threat to public health.
Rapid Escalation in Cases in Paraná's Capital
In just over two months, the capital of Paraná has witnessed a staggering 26-fold increase in daily COVID-19 cases. The Municipal Health Department reports a surge from an average of 27 cases to a concerning 728 cases between the end of 2023 and the beginning of March 2024. Currently, the city is grappling with 5,067 active cases, and in a single day at the end of February, 1,026 new confirmations were recorded - a figure not seen since the close of 2022.
Contributing Factors: End-of-Year Festivities and Carnival
The latest bulletin from the Municipal Health Department, spanning from February 28th to March 5th, reveals a distressing tally of 5,098 new cases and three deaths. Victims, aged between 50 and 88, had comorbidities and an incomplete vaccination schedule. The Municipal Health Department points to end-of-year festivities and Carnival as the catalysts for this new wave of COVID-19, emphasizing the role of large gatherings in facilitating the virus's transmission.
 saude.curitiba.pr.gov.br
saude.curitiba.pr.gov.br
New SARS-CoV-2 Sub-lineages JN.1.7 and JN.2.5 Possible At Play.
According to local experts, the JN.1.7 and JN.2.5 are possibly behind the new surge in Paranas.
The JN.2.5 had already been wreaking in nearby Mato Gross state for a while now.
The JN.1.7 is another new variant that is also rising in circulation across various parts in Brazil.
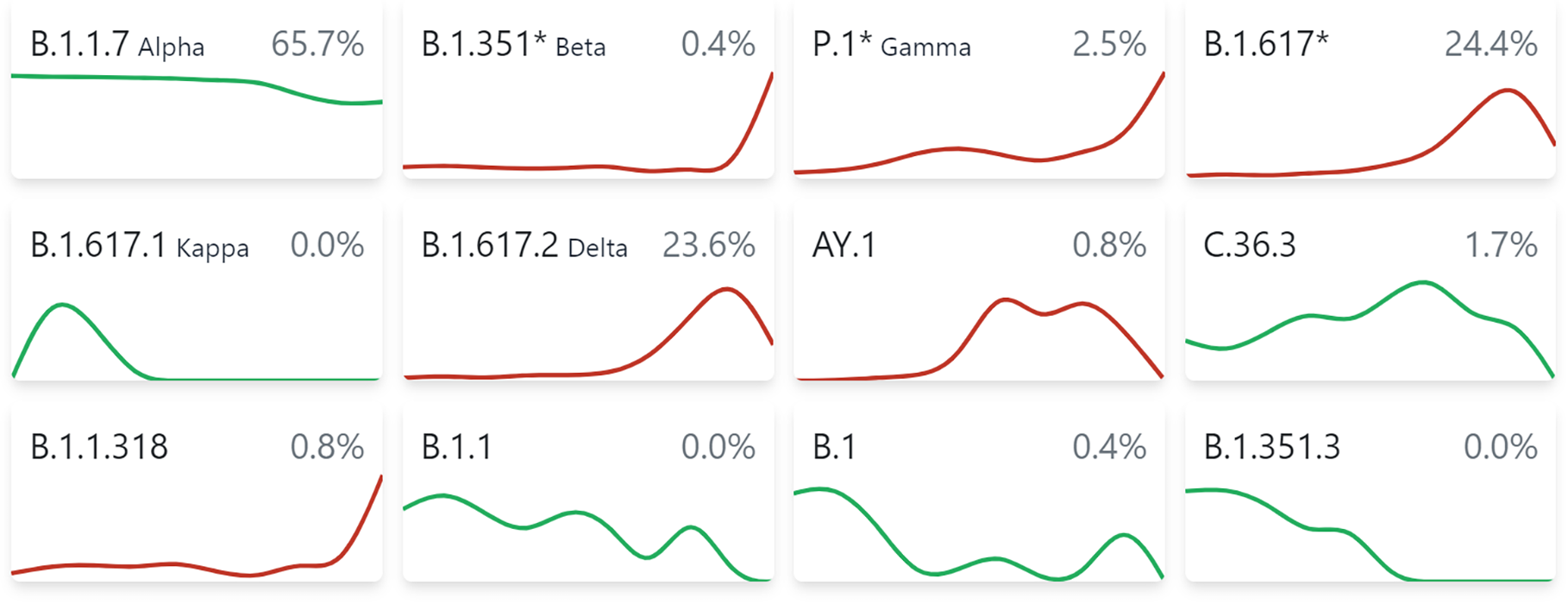
 cov-spectrum.org
cov-spectrum.org
Vaccination Remains the Cornerstone of Defense
Despite the surge, the Municipal Health Department underscores that vaccination remains the primary weapon in the fight against the virus. The department recommends adherence to preventive measures, including the wearing of masks in crowded indoor spaces and regular handwashing. Individuals experiencing respiratory symptoms are advised to don masks, initiate self-isolation, and promptly contact the Central Saúde Já Curitiba for assistance.
Three Years into Vaccination: Changing the Pandemic Landscape
Three years ago, Curitiba initiated its vaccination campaign against COVID-19, marking a significant turning point in the pandemic landscape. The vaccination effort has contributed to a reduction in deaths, providing a semblance of control over the virus. However, the recent surge serves as a stark reminder that the battle against COVID-19 is far from over.
Incomplete Vaccination and Comorbidities Contribute to Fatal Outcomes
In the week between February 28th and March 5th, three deaths were reported in Curitiba, involving individuals aged 50 to 88 with comorbidities and incomplete vaccination schedules. The resurgence is attributed not only to mass gatherings during festivities but also to a false sense of security brought about by the decline in deaths following widespread vaccinations.
Long-Term Coexistence with COVID-19: A Public Health Reality
The municipal secretary of Health, Beatriz Battistella, issues a sobering reminder that living with the COVID-19 virus is an enduring reality. She emphasizes the necessity for ongoing attention to these waves of contamination, urging the public to remain vigilant despite the strides made in vaccination efforts.
Current Impact on Health Infrastructure
As of the latest update, the surge in COVID-19 cases has not yet strained the health network in Curitiba, local health authorities claimed. At 4 pm on March 6th, there was only one patient in an ICU bed and ten in the ward. However, many hospitals cross the state are filled with patient exhibiting severe respiratory issues and have to be classified according to what is causing these infections! Health authorities are also stressing the unpredictability of the situation.
Local COVID-19 News coverages indicate that there is an increasing number of sick individuals with respiratory symptoms seeking outpatient services at various hospitals and clinics across Paranas.
With over 5,000 new cases reported, health authorities in Curitiba issue a stern warning about the imperative need to maintain caution and adherence to preventive measures.
Consistent Recommendations for Public Safety
The familiar refrain resounds: the recommended course of action remains consistent with pandemic guidelines. The public is urged to get vaccinated, wear masks in enclosed spaces and crowded settings, and regularly use alcohol gel to sanitize hands. These preventive measures, while seemingly routine, play a crucial role in mitigating the spread of the virus and protecting public health.
In conclusion, Paraná, Brazil, faces a renewed threat from COVID-19, driven by the emergence of variants and exacerbated by mass gatherings. The recent surge serves as a poignant reminder that, despite advancements in vaccination efforts, the battle against the virus is ongoing. It underscores the importance of sustained vigilance, adherence to preventive measures, and a collective commitment to overcoming the challenges posed by the ever-evolving nature of the pandemic.
Parana, A State In Brazil Currently Inundated With Rising COVID-19 Infections. JN.2.5 And JN.1.7 Variants Possibly At Play
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 07, 2024
The state of Paraná in Brazil finds itself once again grappling with a surge in COVID-19 infections, driven by the emergence of the JN.2.5 and JN.1.7 variants. The Municipal Health Department is sounding the alarm as the number of daily cases has skyrocketed, posing a significant threat to public health.
Rapid Escalation in Cases in Paraná's Capital
In just over two months, the capital of Paraná has witnessed a staggering 26-fold increase in daily COVID-19 cases. The Municipal Health Department reports a surge from an average of 27 cases to a concerning 728 cases between the end of 2023 and the beginning of March 2024. Currently, the city is grappling with 5,067 active cases, and in a single day at the end of February, 1,026 new confirmations were recorded - a figure not seen since the close of 2022.
Contributing Factors: End-of-Year Festivities and Carnival
The latest bulletin from the Municipal Health Department, spanning from February 28th to March 5th, reveals a distressing tally of 5,098 new cases and three deaths. Victims, aged between 50 and 88, had comorbidities and an incomplete vaccination schedule. The Municipal Health Department points to end-of-year festivities and Carnival as the catalysts for this new wave of COVID-19, emphasizing the role of large gatherings in facilitating the virus's transmission.
Com mais de 5 mil novos casos de covid, Saúde alerta para manutenção de cuidados em Curitiba
New SARS-CoV-2 Sub-lineages JN.1.7 and JN.2.5 Possible At Play.
According to local experts, the JN.1.7 and JN.2.5 are possibly behind the new surge in Paranas.
The JN.2.5 had already been wreaking in nearby Mato Gross state for a while now.
The JN.1.7 is another new variant that is also rising in circulation across various parts in Brazil.
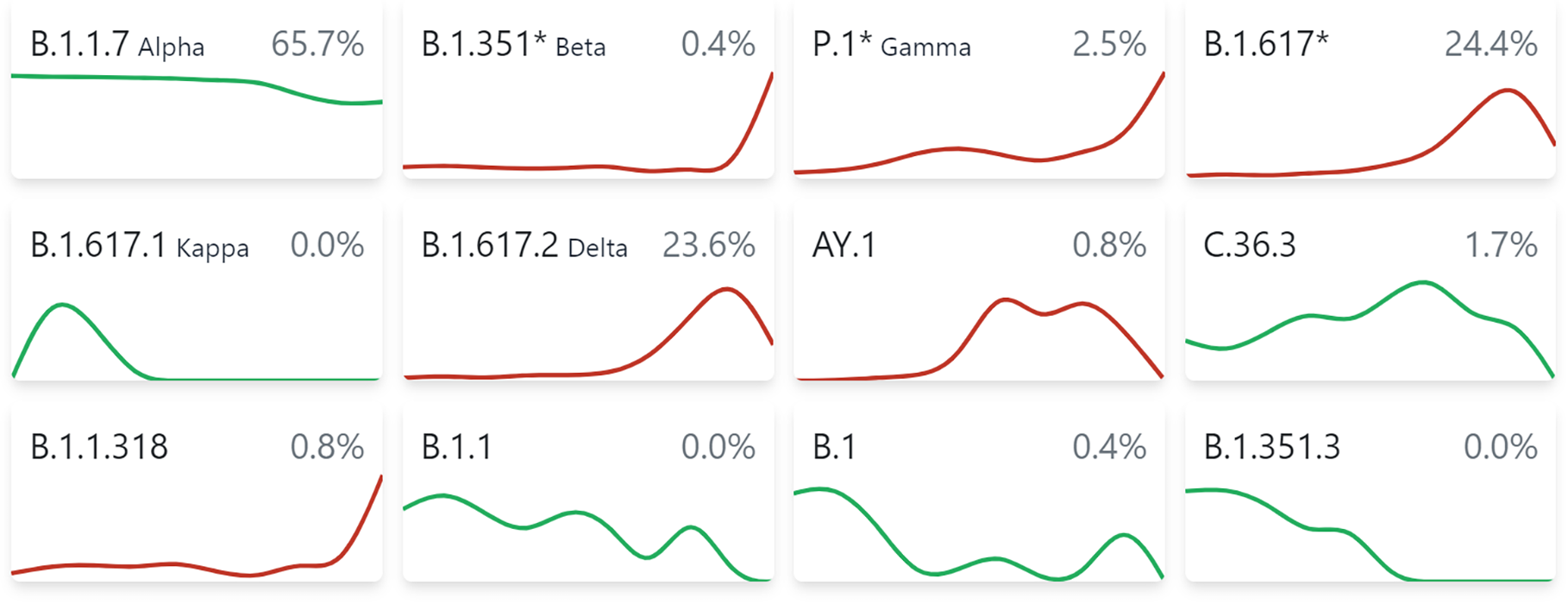
covSPECTRUM
covSPECTRUM is an interactive platform aiming to help scientists investigate and identify variants of SARS-CoV-2.
Vaccination Remains the Cornerstone of Defense
Despite the surge, the Municipal Health Department underscores that vaccination remains the primary weapon in the fight against the virus. The department recommends adherence to preventive measures, including the wearing of masks in crowded indoor spaces and regular handwashing. Individuals experiencing respiratory symptoms are advised to don masks, initiate self-isolation, and promptly contact the Central Saúde Já Curitiba for assistance.
Three Years into Vaccination: Changing the Pandemic Landscape
Three years ago, Curitiba initiated its vaccination campaign against COVID-19, marking a significant turning point in the pandemic landscape. The vaccination effort has contributed to a reduction in deaths, providing a semblance of control over the virus. However, the recent surge serves as a stark reminder that the battle against COVID-19 is far from over.
Incomplete Vaccination and Comorbidities Contribute to Fatal Outcomes
In the week between February 28th and March 5th, three deaths were reported in Curitiba, involving individuals aged 50 to 88 with comorbidities and incomplete vaccination schedules. The resurgence is attributed not only to mass gatherings during festivities but also to a false sense of security brought about by the decline in deaths following widespread vaccinations.
Long-Term Coexistence with COVID-19: A Public Health Reality
The municipal secretary of Health, Beatriz Battistella, issues a sobering reminder that living with the COVID-19 virus is an enduring reality. She emphasizes the necessity for ongoing attention to these waves of contamination, urging the public to remain vigilant despite the strides made in vaccination efforts.
Current Impact on Health Infrastructure
As of the latest update, the surge in COVID-19 cases has not yet strained the health network in Curitiba, local health authorities claimed. At 4 pm on March 6th, there was only one patient in an ICU bed and ten in the ward. However, many hospitals cross the state are filled with patient exhibiting severe respiratory issues and have to be classified according to what is causing these infections! Health authorities are also stressing the unpredictability of the situation.
Local COVID-19 News coverages indicate that there is an increasing number of sick individuals with respiratory symptoms seeking outpatient services at various hospitals and clinics across Paranas.
With over 5,000 new cases reported, health authorities in Curitiba issue a stern warning about the imperative need to maintain caution and adherence to preventive measures.
Consistent Recommendations for Public Safety
The familiar refrain resounds: the recommended course of action remains consistent with pandemic guidelines. The public is urged to get vaccinated, wear masks in enclosed spaces and crowded settings, and regularly use alcohol gel to sanitize hands. These preventive measures, while seemingly routine, play a crucial role in mitigating the spread of the virus and protecting public health.
In conclusion, Paraná, Brazil, faces a renewed threat from COVID-19, driven by the emergence of variants and exacerbated by mass gatherings. The recent surge serves as a poignant reminder that, despite advancements in vaccination efforts, the battle against the virus is ongoing. It underscores the importance of sustained vigilance, adherence to preventive measures, and a collective commitment to overcoming the challenges posed by the ever-evolving nature of the pandemic.
Heliobas Disciple
TB Fanatic

Pathologist reports a stunning 52% increase in cancer risk for ages 15-59 who were vaxxed
I just interviewed a pathologist in Croatia who told me about a study she did which shows a 52% increase in carcinomas (all stages) in ages 15-59 who took the jab. She refuses to be vaxxed
Pathologist reports a stunning 52% increase in cancer risk for ages 15-59 who were vaxxed
I just interviewed a pathologist in Croatia who told me about a study she did which shows a 52% increase in carcinomas (all stages) in ages 15-59 who took the jab. She refuses to be vaxxed
Steve Kirsch
Mar 5, 2024
Executive summary
I just interviewed Ivana Pavic, a pathologist in Croatia.
She did a careful study in Croatia and found that while 55% of the 15 to 59 year olds are vaccinated, 65% of the carcinoma cases in that age group had one or more shots.
If you do the math, it means that the COVID vaccines increased your risk of getting cancer by a whopping 52%. Did they warn you about that before they gave you the shots?
I called up John Beaudoin and he was nonplussed: “I’m surprised it was so low.”
In short, this is a train wreck, and there is no other explanation for this differential since the only difference between the groups was whether they were vaccinated or not.
The full interview can be found here [31 min 58 sec]
The study referenced in the interview:
IN THE POST-PANDEMIC ERA OF COVID: EPIDEMIOLOGICAL COUNTERMEASURES AND THE POTENTIAL OF „MALIGNANT DISEASES EPIDEMIC“
The math
The easiest way to visualize this is you start with 100 people: 55 vax, 45 unvaxxed.
Suppose your cancer risk is 10% for both groups.
Then you’d have 5.5 and 4.5 which is 55% vaxxed.
To get to a 65% ratio, it would mean that more vaxxed people got cancer: 8.342 people.
So you then take 8.342/5.5=1.517.
So a 52% increase over baseline risk.
Summary
Ivana isn’t taking any shots and she doesn’t recommend them for anyone.
She is not alone. Hardly anyone in Croatia is opting for the shots anymore either, even though 99% of the doctors recommend them as safe and effective. Maybe I can get one of them to come on camera with me to explain their recommendation.
Heliobas Disciple
TB Fanatic
New and damning evidence
Dr. John Campbell
Mar 6, 2024
8 min 15 sec
To be reported to the UK police. Read the full letter here
(Letter from Andrew Bridge, member of Parliment, dated Feb 20 2024 to the police in Britain; there is a video embedded in the twitter, it is 46 min 42 sec long.)
View: https://twitter.com/JimFergusonUK/status/1765289139677618585/photo/1
Heliobas Disciple
TB Fanatic

A Man Got the COVID-19 Vaccine 217 Times – This Is What Happened to Him
Researchers at FAU have discovered no negative effects on the immune system. Scientists at Friedrich-Alexander University Erlangen-Nürnberg (FAU) and Erlangen University Hospital have studied a man who has undergone over 200 Covid-19 vaccinations. They learned of his case via newspaper reports. Unt
scitechdaily.com
A Man Got the COVID-19 Vaccine 217 Times – This Is What Happened to Him
By Friedrich-Alexander-Universität Erlangen-Nürnberg
March 7, 2024
A study on a man with over 200 COVID-19 vaccinations revealed a fully functional and even enhanced immune response, debunking the theory that excessive vaccination weakens immunity, as shown in research findings published in The Lancet Infectious Diseases.
Researchers at FAU have discovered no negative effects on the immune system.
Scientists at Friedrich-Alexander University Erlangen-Nürnberg (FAU) and Erlangen University Hospital have studied a man who has undergone over 200 Covid-19 vaccinations. They learned of his case via newspaper reports. Until now, it has been unclear what effects hypervaccination such as this would have on the immune system.
Some scientists were of the opinion that immune cells would become less effective after becoming used to the antigens. This proved not to be the case in the individual in question: his immune system is fully functional. Certain immune cells and antibodies against SARS-CoV-2 are even present in considerably higher concentrations than is the case with people who have only received three vaccinations. The results have been published in the journal The Lancet Infectious Diseases.
More than 60 million people in Germany have been vaccinated against SARS-Coronavirus 2, the majority of them several times. The man who has now been examined by researchers at FAU claims to have received 217 vaccinations for private reasons. There is official confirmation for 134 of these vaccinations.
“We learned about his case via newspaper articles,” explains Privatdozent Dr. Kilian Schober from the Institute of Microbiology – Clinical Microbiology, Immunology and Hygiene (director Prof. Dr. Christian Bogdan). “We then contacted him and invited him to undergo various tests in Erlangen. He was very interested in doing so.” Schober and his colleagues wanted to know what consequences hypervaccination such as this would have. How does it alter the immune response?
As a rule, vaccinations contain parts of the pathogen or a type of construction plan that the vaccinated person’s cells can use to produce these pathogenic components themselves. Thanks to these antigens, the immune system learns to recognize the real pathogen in the event of a later infection. It can then react more rapidly and forcibly. But what happens if the body’s immune system is exposed extremely often to a specific antigen?
“That may be the case in a chronic infection such as HIV or Hepatitis B, that has regular flare-ups,” explains Schober. “There is an indication that certain types of immune cells, known as T-cells, then become fatigued, leading to them releasing fewer pro-inflammatory messenger substances.” This and other effects triggered by the cells becoming used to the antigens can weaken the immune system. The immune system is then no longer able to combat the pathogen so effectively.
Blood samples from several years investigated
The current study, which also involved researchers from Munich and Vienna, does not deliver any indication that this is the case, however. “The individual has undergone various blood tests over recent years;” explains Schober. “He gave us his permission to assess the results of these analyses. In some cases, samples had been frozen, and we were able to investigate these ourselves. We were also able to take blood samples ourselves when the man received a further vaccination during the study at his own insistence. We were able to use these samples to determine exactly how the immune system reacts to the vaccination.”
The results showed that the individual has large numbers of T-effector cells against SARS-CoV-2. These act as the body’s own soldiers that fight against the virus. The test person even had more of these compared to the control group of people who have received three vaccinations. The researchers did not perceive any fatigue in these effector cells, they were similarly effective as those in the control group who had received the normal number of vaccinations.
Memory T cells are another aspect the researchers explored. These are cells at a preliminary stage, before effector cells. Similar to stem cells, these cells can replenish numbers of suitable effector cells. “The number of memory cells was just as high in our test case as in the control group,” explains Katharina Kocher, one of the leading authors of the study. “Overall, we did not find any indication for a weaker immune response, rather the contrary.” In addition, even the 217th vaccination that the man received during the study still had an effect: the number of antibodies against SARS-CoV-2 increased significantly as a result.
Immune system remains active against other pathogens
Further tests indicated that there was no change to the immune system’s effectiveness against other pathogens. It therefore appears to be the case that the hypervaccination has not damaged the immune system as such. “Our test case was vaccinated with a total of eight different vaccines, including different available mRNA vaccines,” stated Dr. Kilian Schober. “The observation that no noticeable side effects were triggered in spite of this extraordinary hypervaccination indicates that the drugs have a good degree of tolerability.”
However, this is one individual case. The results are not sufficient for making far-reaching conclusions let alone recommendations for the general public. “Current research indicates that a three-dose vaccination, coupled with regular top-up vaccines for vulnerable groups, remains the favored approach. There is no indication that more vaccines are required.”
Reference: “Adaptive immune responses are larger and functionally preserved in a hypervaccinated individual” by Katharina Kocher, Carolin Moosmann, Felix Drost, Christine Schülein, Pascal Irrgang, Philipp Steininger, Jahn Zhong, Johannes Träger, Bernd Spriewald, Christoph Bock, Dirk H Busch, Christian Bogdan, Benjamin Schubert, Thomas H Winkler, Matthias Tenbusch, Ev-Marie Schuster and Kilian Schober, 4 March 2024, The Lancet Infectious Diseases.
DOI: 10.1016/S1473-3099(24)00134-8
Heliobas Disciple
TB Fanatic

COVID-19 virus can stay in the body more than a year after infection, research finds
The COVID-19 virus can persist in the blood and tissue of patients for more than a year after the acute phase of the illness has ended, according to new research from UC San Francisco that offers potential clues to why some people develop long COVID.
COVID-19 virus can stay in the body more than a year after infection, research finds
by University of California, San Francisco
March 7 2024
The COVID-19 virus can persist in the blood and tissue of patients for more than a year after the acute phase of the illness has ended, according to new research from UC San Francisco that offers potential clues to why some people develop long COVID.
The scientists found pieces of SARS-CoV-2, referred to as COVID antigens, lingering in the blood up to 14 months after infection and for more than two years in tissue samples from people who had COVID.
"These two studies provide some of the strongest evidence so far that COVID antigens can persist in some people, even though we think they have normal immune responses," said Michael Peluso, MD, an infectious disease researcher in the UCSF School of Medicine, who led both studies.
The findings were presented at the Conference on Retroviruses and Opportunistic Infections (CROI), which was held March 3 to 6, 2024, in Denver, Colorado.
Evidence of long-term infection
Early in the pandemic, COVID-19 was thought to be a transient illness. But a growing number of patients, even those who had previously been healthy, continued having symptoms, such as, brain fog, digestive problems and vascular issues, for months or even years.
The researchers looked at blood samples from 171 people who had been infected with COVID. Using an ultra-sensitive test for the COVID "spike" protein, which helps the virus break into human cells, the scientists found the virus was still present up to 14 months later in some people.
Among those who were hospitalized for COVID, the likelihood of detecting the COVID antigens was about twice as high as it was for those who were not. It was also higher for those who reported being sicker, but were not hospitalized.
"As a clinician, these associations convince me that we are on to something, because it makes sense that someone who had been sicker with COVID would have more antigen that can stick around," Peluso said.
Virus persists up to two years in tissue
Since the virus is believed to persist in the tissue reservoirs, the scientists turned to UCSF's Long COVID Tissue Bank, which contains samples donated by patients with and without long COVID.
They detected portions of viral RNA for up to two years after infection, although there was no evidence that the person had become reinfected. They found it in the connective tissue where immune cells are located, suggesting that the viral fragments were causing the immune system to attack. In some of the samples, the researchers found that the virus could be active.
Peluso said more research is needed to determine whether the persistence of these fragments drives long COVID and such associated risks as heart attack and stroke.
But, based on these findings, Peluso's team at UCSF is involved in multiple clinical trials that are testing whether monoclonal antibodies or antiviral drugs can remove the virus and improve the health of people with long COVID.
"There is a lot more work to be done, but I feel like we are making progress in really understanding the long-term consequences of this infection," Peluso said.
Provided by University of California, San Francisco
Heliobas Disciple
TB Fanatic
(fair use applies)
Higher Dietary Iron And Zinc Intake Are Associated With Decreased Risk Of COVID-19 Infection And Hospitalization
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 08, 2024
The ongoing battle against the global pandemic caused by the novel Coronavirus-disease 2019 (COVID-19) has prompted extensive research into various factors influencing infection susceptibility and severity. Among these, the role of dietary minerals has gained attention, particularly in older adults. This COVID-19 News report delves into a comprehensive study conducted by Mashhad University of Medical Sciences in Iran, exploring the association between dietary mineral intake and the incidence of COVID-19 as well as the subsequent risk of hospitalization.
Understanding the Immune System and Nutrition
The immune system plays a crucial role in protecting individuals from infectious diseases, including COVID-19. Nutrition is a key determinant of immune system function, with essential micronutrients such as zinc, copper, iron, selenium, magnesium, and fatty acids being vital for optimal immune response. Deficiencies in these micronutrients can increase susceptibility to infectious diseases. In the context of COVID-19, a study found that most patients were zinc deficient, leading to more complications, longer hospital stays, and increased mortality.
Complex Dynamics of COVID-19 and Advanced Data Analysis
Due to the complex and dynamic nature of COVID-19, traditional linear analysis methods may not be sufficient to fully understand its intricacies. Nonlinear mathematical approaches, such as dynamic system models, have proven effective in analyzing the interactions, feedback loops, and non-proportional relationships between variables in the context of the pandemic. The study conducted by Mashhad University of Medical Sciences is the first of its kind to employ dynamic system models to predict the relationship between dietary mineral intake and COVID-19 incidence and hospitalization.
Results of the Cohort Study
The study included 1957 participants aged 35 - 65, with dietary intake documented using a validated 65-item food frequency questionnaire (FFQ) since 2007. COVID-19 PCR test results were collected between February 2020 and June 2022. The analysis revealed that dietary intakes of magnesium, iron, and potassium were significantly lower in COVID-19-positive patients. After adjustments for age and sex, dietary iron remained significantly associated with COVID-19 incidence, indicating a 6% reduction in the risk of infection with each unit increase in iron intake.
Furthermore, a significant relationship was observed between dietary zinc and hospitalization due to COVID-19, with a 31% reduction in the relative risk of hospitalization for each unit increase in zinc intake. Dynamic system models identified specific cut-offs for daily consumption of calcium, zinc, and iron, below which an increased risk of COVID-19 incidence was noted.
Discussion of Findings
The study's findings emphasize the significance of dietary mineral intake, specifically iron and zinc, in influencing the risk of COVID-19 infection and subsequent hospitalization. Iron, essential for various enzymatic processes and influencing viral pathogenesis, showed a clear association with decreased COVID-19 incidence. Similarly, zinc, crucial for immune system function, exhibited a notable correlation with reduced hospitalization risk.
Interestingly, the study also highlighted the role of calcium and iodine in COVID-19 susceptibility. While higher calcium intake was associated with decreased COVID-19 risk, an excess of iodine intake was linked to an increased risk, demonstrating the intricate interplay between dietary minerals and viral infections.
Limitations and Future Considerations
Despite the strengths of the study, such as its focus on past dietary intakes and the use of advanced data analysis methods, certain limitations should be acknowledged. The reliance on PCR results for identifying COVID-19 patients may introduce classification bias, as some individuals affected by the virus may not have undergone PCR testing. Additionally, the exclusion of individuals with missing dietary intake data and the lack of consideration for other factors like chronic diseases or dietary changes during the pandemic period may affect the generalizability of the results.
Conclusion
In conclusion, the study conducted by Mashhad University of Medical Sciences sheds light on the crucial role of dietary mineral intake in mitigating the risk of COVID-19 infection and subsequent hospitalization in older adults. Higher intake of iron and zinc was associated with a decreased risk of COVID-19 incidence and hospitalization, respectively. The dynamic system models provided valuable insights into specific cut-offs for calcium, zinc, and iron intake, emphasizing the importance of maintaining adequate levels of these minerals for optimal immune function and resilience against viral infections. As the world continues to grapple with the challenges posed by the COVID-19 pandemic, understanding the impact of nutrition on infection risk becomes increasingly vital for public health strategies.
The study findings were published in the peer reviewed journal: BMC Nutrition.

 link.springer.com
link.springer.com
Higher Dietary Iron And Zinc Intake Are Associated With Decreased Risk Of COVID-19 Infection And Hospitalization
Nikhil Prasad Fact checked by:Thailand Medical News Team
Mar 08, 2024
The ongoing battle against the global pandemic caused by the novel Coronavirus-disease 2019 (COVID-19) has prompted extensive research into various factors influencing infection susceptibility and severity. Among these, the role of dietary minerals has gained attention, particularly in older adults. This COVID-19 News report delves into a comprehensive study conducted by Mashhad University of Medical Sciences in Iran, exploring the association between dietary mineral intake and the incidence of COVID-19 as well as the subsequent risk of hospitalization.
Understanding the Immune System and Nutrition
The immune system plays a crucial role in protecting individuals from infectious diseases, including COVID-19. Nutrition is a key determinant of immune system function, with essential micronutrients such as zinc, copper, iron, selenium, magnesium, and fatty acids being vital for optimal immune response. Deficiencies in these micronutrients can increase susceptibility to infectious diseases. In the context of COVID-19, a study found that most patients were zinc deficient, leading to more complications, longer hospital stays, and increased mortality.
Complex Dynamics of COVID-19 and Advanced Data Analysis
Due to the complex and dynamic nature of COVID-19, traditional linear analysis methods may not be sufficient to fully understand its intricacies. Nonlinear mathematical approaches, such as dynamic system models, have proven effective in analyzing the interactions, feedback loops, and non-proportional relationships between variables in the context of the pandemic. The study conducted by Mashhad University of Medical Sciences is the first of its kind to employ dynamic system models to predict the relationship between dietary mineral intake and COVID-19 incidence and hospitalization.
Results of the Cohort Study
The study included 1957 participants aged 35 - 65, with dietary intake documented using a validated 65-item food frequency questionnaire (FFQ) since 2007. COVID-19 PCR test results were collected between February 2020 and June 2022. The analysis revealed that dietary intakes of magnesium, iron, and potassium were significantly lower in COVID-19-positive patients. After adjustments for age and sex, dietary iron remained significantly associated with COVID-19 incidence, indicating a 6% reduction in the risk of infection with each unit increase in iron intake.
Furthermore, a significant relationship was observed between dietary zinc and hospitalization due to COVID-19, with a 31% reduction in the relative risk of hospitalization for each unit increase in zinc intake. Dynamic system models identified specific cut-offs for daily consumption of calcium, zinc, and iron, below which an increased risk of COVID-19 incidence was noted.
Discussion of Findings
The study's findings emphasize the significance of dietary mineral intake, specifically iron and zinc, in influencing the risk of COVID-19 infection and subsequent hospitalization. Iron, essential for various enzymatic processes and influencing viral pathogenesis, showed a clear association with decreased COVID-19 incidence. Similarly, zinc, crucial for immune system function, exhibited a notable correlation with reduced hospitalization risk.
Interestingly, the study also highlighted the role of calcium and iodine in COVID-19 susceptibility. While higher calcium intake was associated with decreased COVID-19 risk, an excess of iodine intake was linked to an increased risk, demonstrating the intricate interplay between dietary minerals and viral infections.
Limitations and Future Considerations
Despite the strengths of the study, such as its focus on past dietary intakes and the use of advanced data analysis methods, certain limitations should be acknowledged. The reliance on PCR results for identifying COVID-19 patients may introduce classification bias, as some individuals affected by the virus may not have undergone PCR testing. Additionally, the exclusion of individuals with missing dietary intake data and the lack of consideration for other factors like chronic diseases or dietary changes during the pandemic period may affect the generalizability of the results.
Conclusion
In conclusion, the study conducted by Mashhad University of Medical Sciences sheds light on the crucial role of dietary mineral intake in mitigating the risk of COVID-19 infection and subsequent hospitalization in older adults. Higher intake of iron and zinc was associated with a decreased risk of COVID-19 incidence and hospitalization, respectively. The dynamic system models provided valuable insights into specific cut-offs for calcium, zinc, and iron intake, emphasizing the importance of maintaining adequate levels of these minerals for optimal immune function and resilience against viral infections. As the world continues to grapple with the challenges posed by the COVID-19 pandemic, understanding the impact of nutrition on infection risk becomes increasingly vital for public health strategies.
The study findings were published in the peer reviewed journal: BMC Nutrition.

Dietary mineral intakes predict Coronavirus-disease 2019 (COVID-19) incidence and hospitalization in older adults - BMC Nutrition
Background The aim of this study was to determine the association between dietary mineral intake and Coronavirus-disease 2019 (COVID-19) infection and its associated hospitalization. Methods This cohort study utilized the MASHAD study population, which comprised individuals aged 35–65. Upon...
wobble
Veteran Member
Last edited:
Tristan
Has No Life - Lives on TB
View: https://www.youtube.com/watch?v=wXcMhWEjkqE
New and damning evidence
Dr. John Campbell
Mar 6, 2024
8 min 15 sec
To be reported to the UK police. Read the full letter here
(Letter from Andrew Bridge, member of Parliment, dated Feb 20 2024 to the police in Britain; there is a video embedded in the twitter, it is 46 min 42 sec long.)
View: https://twitter.com/JimFergusonUK/status/1765289139677618585/photo/1
1/3 of the way into Ferguson's interview of Andrew Bridgen, and so far it's definitely worth the time!
"The Gamekeepers are owned by the Poachers!"
And they discuss the Government's effort to jigger the Statistics to make the indications (excess deaths) look better.
Cover Up!
Last edited:
Heliobas Disciple
TB Fanatic

Dangerous strep bacterial infections on pace to hit new record high in Japan - The Mainichi
TOKYO -- Rapidly progressing and known for their 30-70% fatality rate, acute hemolytic streptococcal bacterial infections are spreading in Japan at a
Dangerous strep bacterial infections on pace to hit new record high in Japan
March 6, 2024 (Mainichi Japan)
Japanese version
TOKYO -- Rapidly progressing and known for their 30-70% fatality rate, acute hemolytic streptococcal bacterial infections are spreading in Japan at a quicker pace than in 2023, which itself saw a record high number of cases.
The number of patients in the country has already reached 40% of last year's total within the first two months of 2024. Although the background reasons for the spread remain unclear, the health ministry is intensifying monitoring by investigating strains known for their pathogenicity and infectiousness.
According to provisional figures from the National Institute of Infectious Diseases, there were 941 hemolytic streptococcus cases reported nationwide last year. The number of patients has continued to increase this year, reaching 378 as of Feb. 25. Cases have been confirmed in 45 of Japan's 47 prefectures, with only Akita and Iwate recording zero.
Group A hemolytic streptococcus, which causes sore throats mainly in children, is a representative example among several pathogenic bacteria. Although infections often present similar symptoms to a cold, in rare cases and regardless of age, they can escalate to severe conditions including strep throat, tonsillitis, pneumonia and meningitis. Once the infection becomes acute, it can cause multiple organ failure and necrosis in tissue surrounding the muscles.
According to the health ministry, it is unknown how infections escalate. However, the prevalence of sore throats among children since last summer is cited as a contributing factor in the increase in severe cases. Additionally, strains within Group A streptococcus known for their high pathogenicity, already widely reported in Britain, have also been confirmed domestically. In January, the ministry asked local governments to analyze strains collected from acute cases.
The ministry emphasizes that basic infection control measures such as hand hygiene and cough etiquette are crucial, as the infection spreads through droplets or contact between people.
(Japanese original by Ayami Abe, Lifestyle, Science & Environment News Department)

