(fair use applies)
SARS2 vaccination is encouraging steadily more virulent new Omicron variants to evolve
Radagast
February 28, 2024
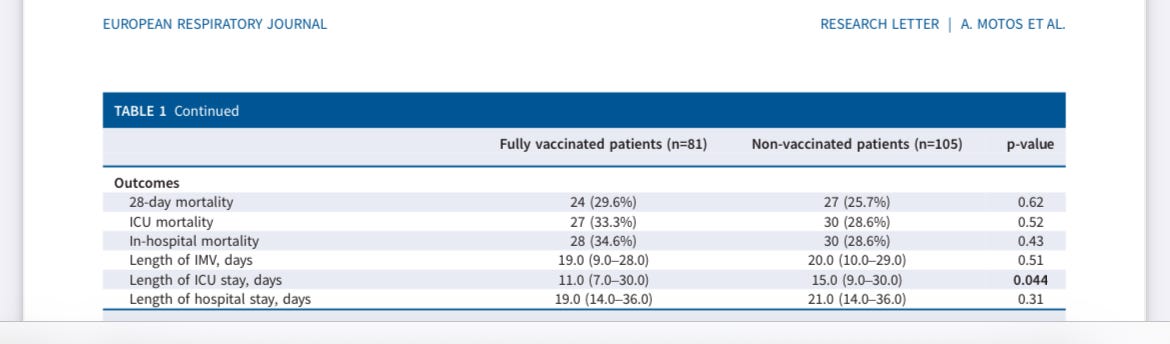
When you vaccinate people against a virus they’re subsequently going to get infected by twice a year or more, then you want the induced immune response to be suitable for the long term. Everything suggests however, that the SARS2 vaccines induce an immune response that is not suitable for the long term. This is not just problematic for the people who received these vaccines, it is problematic because it is encouraging the evolution of more virulent SARS2 variants, as I will demonstrate in this post.
This is an important post, where I will explain three important points in successive order:
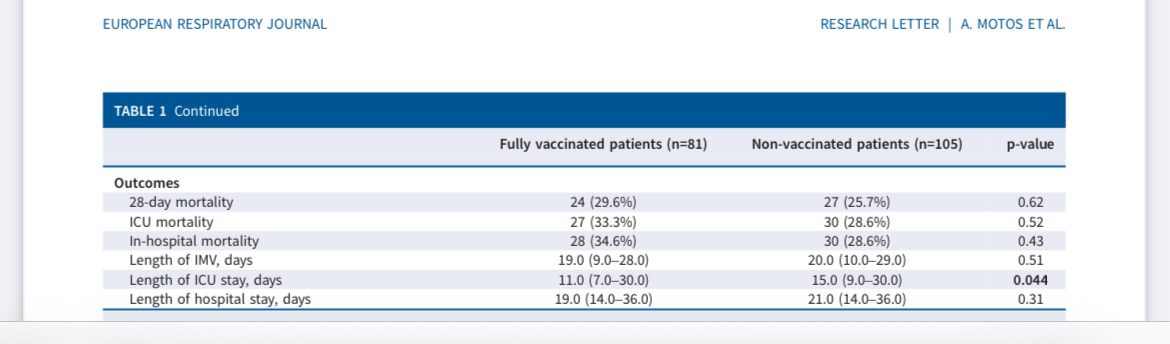
- Vaccination has induced an inappropriate immune response to SARS2, that damages the body. Experts who observe this inappropriate immune response in patients are now openly calling in the scientific literature for an end to the use of these vaccines.
- The inappropriate immune response has started encouraging the evolution of successively more virulent variants of SARS2, ever since the first Omicron variants emerged. This is in contrast to the natural immune response, which selects against virulence.
- We can identify the molecular changes that will encourage a dramatic increase in virulence. These are mutations that would normally fail to spread themselves, but are now starting to be selected because of very strong antibody pressure on a specific region of the Spike protein and likely facilitated by the unique new insertion mutation seen in BA.2.86.
The immune system has various tools in its repertoire, with which to deal with an infection. When the immune response to a pathogen is overly aggressive, this can be deadly or result in excessive damage to the body.
An important principle to understand, is that your cells are not just passive victims upon infection by a virus like SARS2. These cells can be instructed by various signaling molecules to remove viral material that has infected them, or they can use specialized receptors, to figure out on their own they have been infected. Upon instruction by immune cells,
OAS1 can be activated, which degrades the RNA within a cell. RIG-1 receptors and similar genes like MDA5 are also meant to recognize viral RNA. Cells
get better at using these pathways, after they’ve been encouraged to use them before.
As I
have explained before, the innate immune system is instrumental in encouraging the cells to deal with viral material that has infected them. It secretes interferons, which directly interfere in the viral replication and assembly process, but also alert a cell that it needs to make sure it’s not infected itself. Dealing with the problem on its own, allows a cell to avoid the fate of being destroyed by the immune system.
This matters, because we’re dealing with a virus that is continually reinfecting most of the population, multiple times a year. We can see that people are
suffering an accelerated decline in their lung function, that continues between 6 and 24 months after suffering a SARS2 infection. If those people then die five years later of COPD, we won’t count them as SARS2 deaths.
And please remember: We gave these vaccines to people of all ages. The response the immune system developed against SARS2 after vaccination, will be continually recalled, for decades to come.
Note also, another problem I have remarked upon before: A steady increase in Dutch people going to their doctor, complaining of a persistent cough:

This problem appears to be getting worse, as the years go by.
And so you’ll have to forgive me, when I insist on delving into the esoteric details of the consequences of this global experiment. When you get this wrong, which they did, the result can be a catastrophe.
I have explained many of the different problems we see, most notoriously the persisting IgG4 response seen in people who received at least 2mRNA vaccines before ever being naturally infected. But this is far from the only problem we’re dealing with.
An important finding you’ll encounter in the literature, is that the T cells induced by vaccination generally don’t secrete interferon Gamma. Interferon Gamma is
highly effective against SARS2, it’s one of the main toolkits your immune cells have developed against viruses and importantly, it allows your infected cells to get rid of a viral infection themselves, without having to be removed by your immune cells.
Over time, with successive infections, you would have more and more cells in your lung environment, that have gone through an infection and know how to deal with it. this doesn’t happen, if your T cells fail to secrete interferon Gamma and your immune system depends instead on simply killing the affected cells.
And
look what the literature teaches us:
In the present study, we also analyzed certain aspects of the cellular immune response in the three different cohorts described above. This included for one part the IFN-γ secretory response of pan T cells specific for an array of wild type SARS-CoV-2 spike peptides. No significant correlations were found between IFN-γ secretion and neutralization capacities, neither against wild type SARS-CoV-2 nor against the Omicron or Delta variants. Nevertheless, overall IFN-γ secretion significantly increased after booster vaccination with BNT162b2 (Supplementary Figure 3A) and showed a significant correlation with anti-spike IgG titers (Supplementary Figure 3B). Comparison of the three different cohorts demonstrated that no one in the COVID-19-naïve cohort was able to mount a strong IFN-γ response above 4×103 mIU/ml before their third vaccination, while after vaccination a low, but significant 18% of individuals reached such levels (Figure 5A). In contrast, in the COVID-19-convalescent cohorts the percentages of individuals with strong IFN-γ response (> 4×103 mIU/ml) before third vaccination ranged between 31 and 42%, and reached between 50 and 62% after third vaccination (Figure 5A).
With this graph:

You can see in the graph above, that there’s a whole demographic of people who were vaccinated before infection, with Interferon Gamma stuck at a flat 1.
This study also found the same result.
We have somewhat of a clue, as to why the T cells are not releasing Interferon Gamma: Antibodies. Interferon Gamma secretion by T cells is
more pronounced in people without antibodies against Spike.
When antibodies are stuck close together on a particular immunogenic protein, complement can bind to those antibodies. This is something I
have explained before.
Look at this graph:

You can see here that antibodies after vaccination are targeted at specific regions. Because those antibodies are stuck close together on a protein, complement can bind. Hence we see that
complement activation is much stronger after vaccination.
Complement does multiple things. One of the things it does is instruct the innate immune system to destroy a cell. This sounds nice, but isn’t, as it has the ability to be highly damaging to host tissues. There is a state of constant abnormal activation of the adaptive arm of the immune response, in the form of high levels of antibodies that react with every variant of SARS2 circulating in the population.
The outcome you’re effectively dealing with as a result, is that this adaptive immune response is constantly forcing the innate immune system to proceed with killing infected cells, instead of these infected cells receiving an opportunity to solve the problem by removing viral RNA for themselves, learning in the process how to effectively protect themselves from future encounters with the virus.
The other problem of course, is that this type of response is not fast. Waiting for antibodies to bind to SARS2 peptides expressed by a cell, waiting for complement to bind to those antibodies, waiting for complement to trigger a response that destroys the cell membrane, or attracts macrophages and neutrophils to kill the cell, all of this takes time. If those antibodies are IgG4 antibodies, they first need to rise to very high concentrations, for complement to bind.
As always, I’m all in favor of people just reading what I am explaining here and trying to falsify it. Complement is mostly meant for things like destroying toxins, venom and bacteria, harmful agents that breach your natural immune barriers to enter your body and have long stretches of amino acids where they look very different from your own cells.
Antibodies can bind there close to each other and then your immune system can deal with the problem, by binding complement to those antibodies. I have seen nothing to suggest that you would normally deploy complement against a respiratory virus that shows up in your lungs, but feel free to show me an example if you can.
Importantly, complement doesn’t bind to IgA antibodies, only to IgM and IgG. IgA is found in your mucous membranes covering your respiratory tract. But vaccinating people, means IgG starts to compete with IgA and increasingly takes over its job from it. This is why the difference in complement activity is probably even higher in the mucous membranes, than in blood.
And that helps explain why you see
this:

And equally important, why we gradually see
more and more persistent infections emerge in the population:
We identified 381 persistent infections with sequences spanning at least 26 days (11 Alpha, 106 Delta, 97 BA.1 and 167 BA.2). The relatively low number of persistent infections that we identified for Alpha is probably because fewer individuals were infected with Alpha than the other major lineages, but also because a smaller proportion of positive samples with Ct ≤ 30 were sequenced before December 2020, which captures the beginning of the Alpha wave, than after this date (see supplementary figure S1 in ref. 22). Of all the persistent infections that we identified, 54 spanned at least 56 days (3 Alpha, 13 Delta, 15 BA.1 and 23 BA.2).
It’s not just that the number of infections is increasing. As I
explained long ago, infections will increasingly become chronic, as the virus evolves to persist and the immune response is increasingly mismatched.
If you understand all of this, you also understand why the
constant recall of the antibody response is so nasty. Everytime the antibodies are recalled, the adaptive arm of the immune system tells the innate arm to kill the infected cells, rather than infected cells receiving an opportunity to fix the problem themselves and learn in the process.
Why are people’s lungs degrading at an accelerated pace? Well, their immune systems are constantly deploying an adaptive immune response against a virus, that is normally meant to deal with severe infections the innate immune system was unable to reign in on its own. Remember, the first waves of SARS2 failed to result in any detectable antibodies in at least half of those infected, thereby resulting in excessively high estimates of its deadliness, as far more people had already been exposed to it than people thought.
If you’ll forgive me for using a metaphor, imagine if every time people riot after a soccer contest, the police immediately start shooting, rather than first using their batons and resorting to tear gas if things escalate. Yes, the riots will stop, but it’s not a sustainable way of dealing with the problem.
We have an innate immune system for a reason, that picks the tools it picks for a reason. All of this would have been academic, if these vaccines had delivered what they were promised to do: Protection from infection. But they don’t achieve this and more importantly, don’t even turn their recipients into dead-end hosts.
So why isn’t anyone serious warning about any of this? Why do you have to find out about this stuff through an obscure Dutch blog? Well, more and more people are willing to speak out. I’m going to quote a study looking at antibody responses that
was released a month ago:
Knowing that the mRNA vaccines do not prevent infections, the Omicron subvariants have been shown to be less pathogenic, and IgG4 levels have been associated with immunotolerance and numerous negative effects, the recommendations for the successive administration of booster vaccinations to people should be revised.
We’ve finally reached the “saying the quiet part out loud” stage. Millions of people have died by now. Millions more are brain-damaged, or disabled in other ways. The United States has
2.7 million more retired people since 2020 than expected, at least partly due to sickness.
I’ve told you many times now, that this IgG4 dominant response to Spike is a very bad thing.
Importantly, it selects for variants of SARS2 that are more fusogenic, because these antibodies generally fail to instruct the immune system to destroy infected cells, unless they reach the high concentrations that allow complement to bind.
This allows the virus to spread in people’s lungs, by simply fusing infected cells together with neighboring cells. That’s the sort of response we encourage this virus to develop, when we depend on an adaptive immune response that is able to neutralize viral particles, but prohibits the innate immune system from using its tools that enable it to rapidly deal with infected cells.
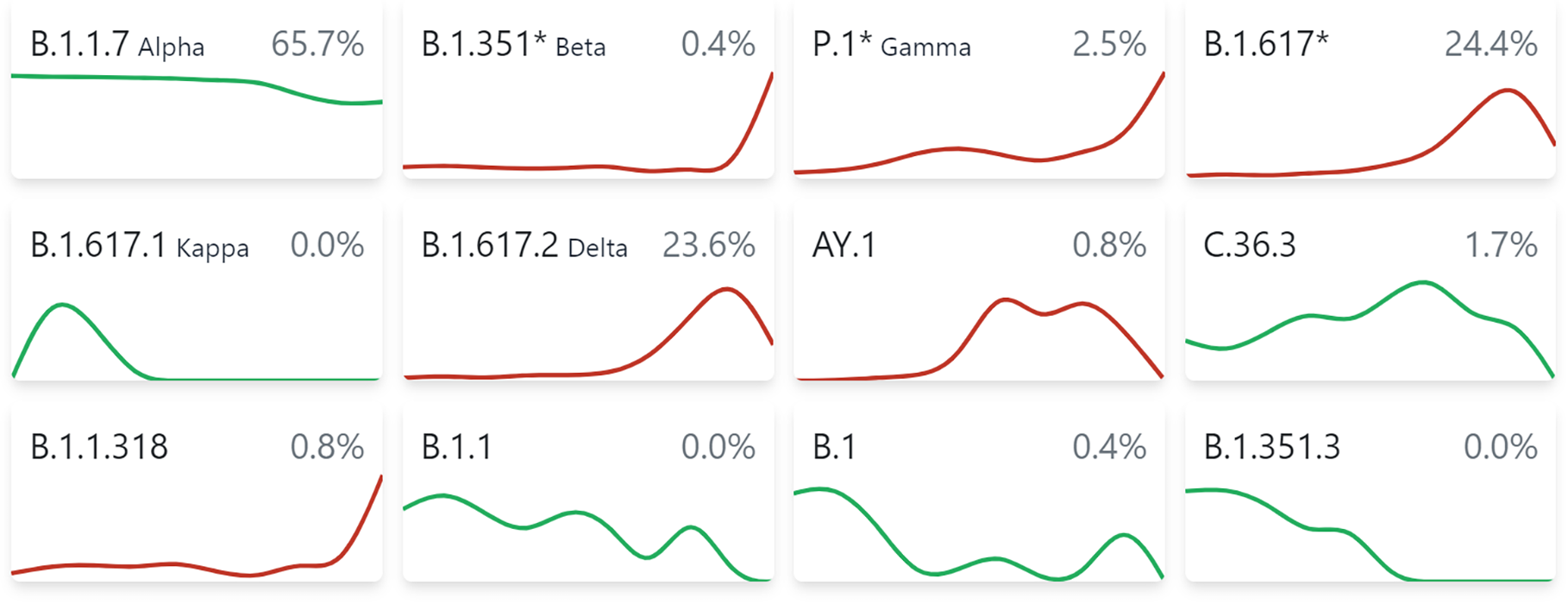
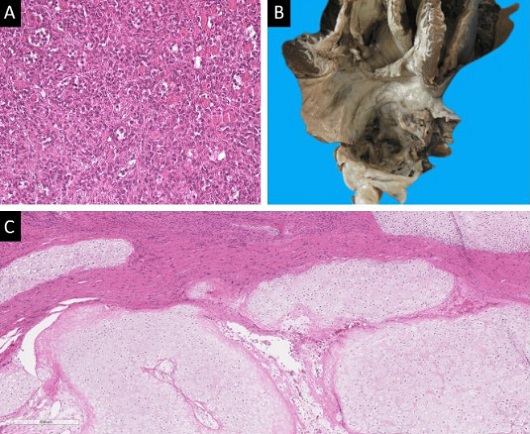
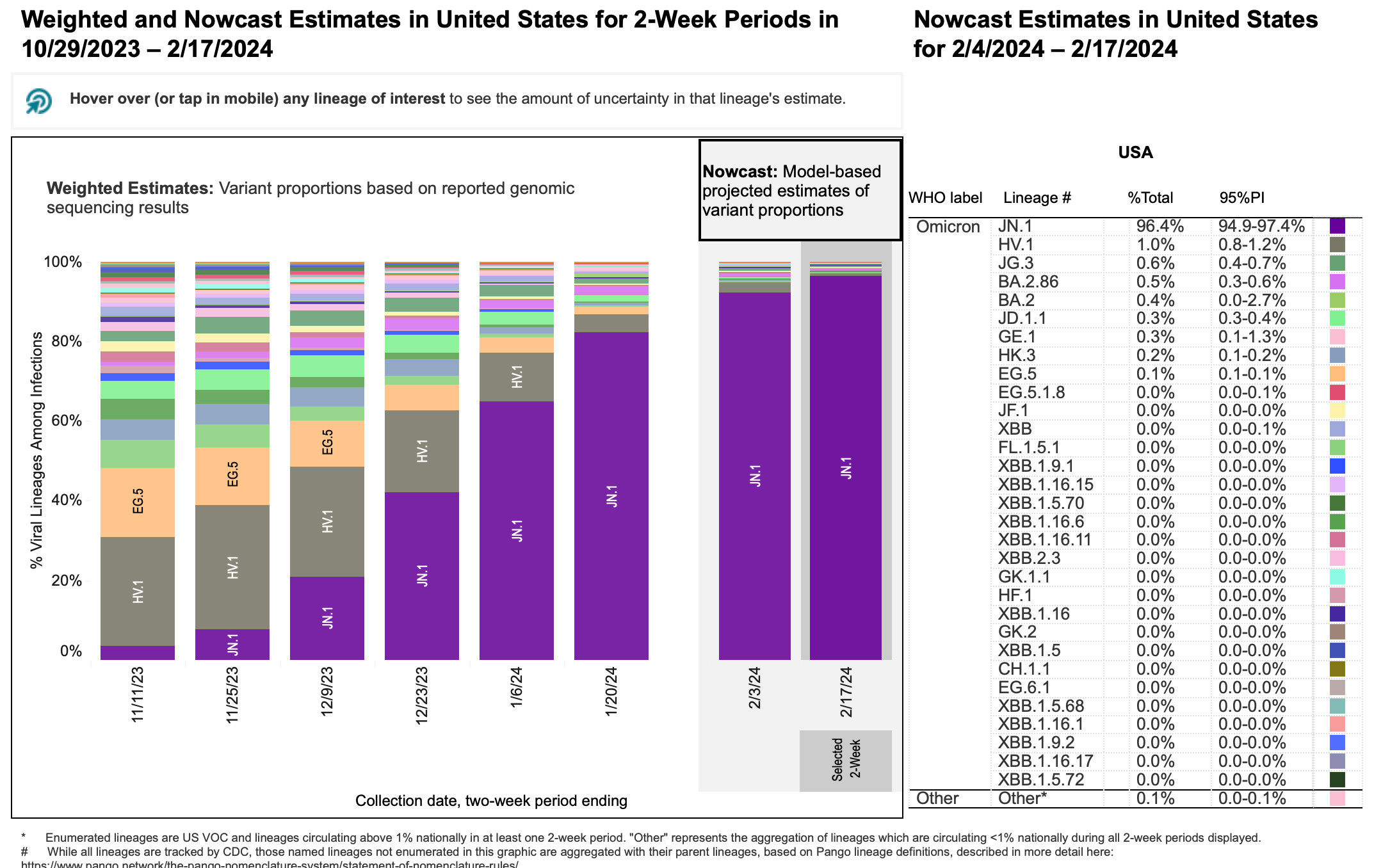
So have a look with me, at the
fusogenicity we see of successive variants in Calu-3 cells, the best available model for the sort of endothelial cells in the lungs this virus hurts:

And
here you see the same result, also in CaLu-3 cells:

It’s not difficult to interpret these results, the trend is obvious. They show that ever since the first two Omicrons (BA.1 and BA.2), the virus is getting slowly but steadily better at fusing cells together, reaching the level seen in the pre-Omicron versions.
That’s what you get, when you force the adaptive immune system to do a job meant for the innate immune system. Fusogenicity is the main determinant of intrinsic virulence we know of. And so, we arrive at the conclusion that we’re encouraging the evolution of ever more virulent variants of this virus.
Why we’re failing to discriminate against virulence
NK cells select against virulence, because these highly fusogenic Spike proteins, with high ACE2 affinity and a positive charge in their RBD, will bind very tightly to the NK cell’s specialized receptors meant to detect the proteins respiratory viruses use to bind to their preferred target cell’s receptors. In addition, the population’s evolving antibody response would normally select against virulence, because people would develop a stronger antibody response to virulence associated epitopes.
Your immune system is not just tasked with protecting you from disease. It’s also an essential part of its job, to discourage the evolution of growing virulence in whatever respiratory viruses you encounter. Otherwise, there would not be eight billion of us right now. As I have explained before, it has been documented for Influenza that
NK cells preferentially bind to the Hemagluttinin genes of highly pathogenic variants of Influenza, like the 1918 flu.
Your IgG3 antibodies are generally cross-reactive, they are capable of binding to multiple different viruses. The job of these antibodies is not so much to protect you from future reinfection by a virus. Rather, the main job of these antibodies is to discriminate against certain virulence-associated epitopes observed in a virus that is circulating in your species.
Why did the 1918 flu not lead to endless waves of severe disease and death? Because of the NK cells that discriminate against it, but also because the survivors of that pandemic
continued to produce very high affinity neutralizing antibodies for decades, that actively discriminated against the virulence associated epitopes of this particular variety of influenza. The survivors did not have long-term immunity from reinfection by influenza. Rather, they had long-term immunity against that particular highly virulent strain, which now had a reproductive disadvantage in our species as a result.
This is not very difficult to understand. It makes perfect sense that one of the many jobs of our immune system is to discriminate against virulent varieties of the hundreds of respiratory viruses known to infect our species. That also perfectly fits the accelerated decline of the more generalist innate immune system, compared to the adaptive immune system: One of the jobs of our elderly, is to use their acquired knowledge to discriminate against virulent pathogens circulating in our species, like the survivors of the 1918 flu did so well for us.
It seems as if nobody ever bothered asking why those previous four hCovs that jumped into our species never wiped us out, before deciding to launch this vaccine.
[CONTINUED NEXT POST]