According to Johns Hopkins Medicine, BRAF is a gene found on chromosome seven that encodes a protein also called BRAF. This protein plays a role in cell growth by sending signals inside the cell that promote, among other functions, cell division. When there is a mutation in the BRAF gene, it creates an abnormal protein that sends erroneous signals that lead to uncontrolled cell growth and cancer. When a person has BRAF-positive melanoma, it means their cancer may grow more aggressively. In 40–50% of the patients with advanced melanoma, BRAF gene mutations are present. Interestingly, the BRAF gene mutation is most likely not inherited, which means that most likely an environmental factor led to the mutation.
The following Case Report is from a 63 yr old man who was initially diagnosed with BRAF-positive maliginant melanoma in 2020. Chemotherapy put him into remission but the cancer came back in 2023, which is when he tried a different approach using fenbendazole.
Q: How old are you? Weight? How do you feel?
A: 63 years old, 232 lb. when this started. About 170 lbs now and gaining my weight back, which is good. I feel wonderful!
Q: What brand of fenbendazole were you taking? And how many times per day? Any side effects?
A: It is TheLife brand of fenbendazole, and my wife bought it on Amazon. I took 222 mg once or twice a day. There were no side effects from the fenben. FYI I saw the health insurance bill for the immunotherapy drug, opdivo, it was $72,000. My wife spent $60 on the fenbendazole, which is what worked!
Q: Are you still taking fenben?
A: Yes. I take 222 mg once per day.
Summary
Congratulations to J. F. for taking matters into his own hands and having a tremendous outcome. We wish him the best going forward and are greatly appreciative of his sharing his experiences so that others faced with similar circumstances may benefit.
BRAF mutations are not restricted to melanomas alone. Again, according to Johns Hopkins, the cancers associated with the BRAF gene mutation are not specific to one part of the body or a certain cell type and include hairy cell leukemias, non-Hodgkin lymphomas, thyroid cancer, ovarian cancer, lung adenocarcinoma, colorectal cancer and certain brain cancers, including glioblastoma, pilocytic astrocytoma, and pediatric low-grade glioma.
In this Case Report, a very aggressive BRAF-positive variant of melanoma appears to have been eradicated by fenbendazole. This report is yet another example of fenbendazole eradicating purported “aggressive” forms of untreatable cancers including triple-negative breast cancers as we’ve previously reported. These results in humans should not be surprising given the wealth of pre-clinical animal data on fenbendazole and mebendazole indicating that these outcomes are to be expected (Doudican, et al., 2013; Simbulan-Rosenthal, et al., 2017 for example, regarding melanomas).
Because J. F. did receive another treatment there could be alternative explanations for his tremendous outcome. First, J. F. did receive two doses of immunotherapy (nivolumab). It is a possibility that that protocol was effective for him in eradicating his BRAF-positive melanoma. Unique individual differences aside, such an outcome would be highly unlikely given the published data on nivolumab as well as J. F.’s oncologist’s expectations and advice.
Second, it is possible that there was an interaction between the two doses of nivolumab, and fenbendazole resulting in a synergistic effect that eradicated the cancer. If this is what happened, it is a major discovery to be further investigated.
Third, fenbendazole alone was the effective anti-cancer agent that eradicated the BRAF-positive melanoma cells. Skimming through the twenty or so references below examining fenbendazole/mebendazole’s role in cancer treatment, indicates that fenbendazole is both necessary and sufficient to achieve the results in experimental pre-clinical models of cancer that J. F. obtained in his own self-treatment cancer clinical trial.
Because the BRAF gene mutation is most likely caused by an environmental factor that led to the mutation, presuming that the factor responsible for the mutation can be eliminated, the possibility of a true cure for BRAF-positive cancers using fenbendazole may be at hand. More on this idea later as we present a more complete discussion as to what cancer is and isn’t in the context of an agent like fenbendazole.
References
Bai RY, Staedtke V, Rudin CM, Bunz F, Figgins GJ. Effective treatment of diverse medulloblastoma models with mebendazole and its impact on tumor angiogenesis. NeuroOncology. 2015; 17:545-54.
Chiang RS, Syed AB, Wright JL, Montgomery B, Srinivas S. Fenbendazole enhancing anti-tumor effect: A case series. Clin. Oncol. Case Rep. 2021; 4:2.
Dobrosotskaya IY, Hammer GD, Schteingart DE, Maturen KE, Worden FP. Mebendazole monotherapy and long-term disease control in metastatic adrenocortical carcinoma. Endocr. Pract. 2011; 17(3):e59-e62.
Doudican NA, Byron AA, Pollock PM, Orlow SJ. XIAP downregulation accompanies mebendazole growth inhibition in melanoma xenografts. Anti-Cancer Drugs. 2013; 24:181-8.
Gallia GL, Holdhoff M, Brem H, Joshi AD, Hann CL, Bai RY, et al. Mebendazole and temozolomide in patients with newly diagnosed high-grade gliomas: results of a phase 1 clinical trial. Neuro- Oncology Advances. 2021; 3:1-8.
Guerini AE, Triggiani L, Maddalo M, Bonu ML, Frassine F, Baiguini A, Alghisi A. Mebendazole as a candidate for drug repurposing in oncology: An extensive review of current literature. Cancers. 2019; 11:1284.
Meco D, Attina G, Mastrangelo S, Navarra P, Ruggiero A. Emerging perspectives on the antiparasitic Mebendazole as a repurposed drug for the treatment of brain cancers. Int. J. Mol. Sci. 2023; 24:1334.
Nygren P, Larsson R. Drug repositioning from bench to bedside: tumor remission by the antihelmintic drug mebendazole in refractory metastatic colon cancer. Acta Oncol. 2014; 53(3):427-8.
Nygren P, Fryknas M, Agerup B, Larsson R. Repositioning of the anthelmintic drug mebendazole for the treatment for colon cancer. J. Cancer res. Clin. Oncol. 2013; 139:2133-40.
Pantziarka P, Bouche G, Meheus L, Sukhatme V, Sukhatme VP. Repurposing drugs in oncology (ReDO) - mebendazole as an anti-cancer agent. Ecancer. 2014; 8:443.
Patel, H., Yacoub, N., Mishra, R., White, A., Long, Y., Alanazi, S., & Garrett, J. T. (2020). Current Advances in the Treatment of BRAF-Mutant Melanoma. Cancers, 12(2), 482.
Pinto LC, Soares BM, de Jusus Viana Pinheiro J, Riggins GJ, Assumpcao PP, Burbano RM, Montenegro RC. The anthelmintic drug mebendazole inhibits growth, migration and invasion in gastric cancer cell model. Toxicology in Vitro. 2015; 29:2038-44.
Pinto LC, de Fatima Aquino Moreira-Nunes C, Soares BM, Rodriguez Burbano RM, de Lemos JA, Montenegro R. Mebendazole, an antiparasitic drug, inhibits drug transporters expression in preclinical model of gastric peritoneal carcinomatosis. Toxicology in Vitro. 2017; 43:87-91.
Sasaki JI, Ramesh R, Chada S, Gomyo Y, Roth JA, Mukhopadhyay T. The anthelmintic drug mebendazole induces mitotic arrest and apoptosis by depolymerizing tubulin in non-small cell lung cancer cells. Molecular Cancer Therapeutics. 2002; 2:1201-9.
Simbulan-Rosenthal CM, DDakshanamurthy S, Gaur A, Chen YS, Fang HB, Abdussamad M, et al. The repurposed anthelmintic mebendazole in combination with trametinib suppresses refractory NRASQ61k melanoma. Oncotarget. 2017; 8:12576-95.
Tan Z, Chen L, Zhang S. Comprehensive modeling and discovery of mebendazole as a novel TRAF2- and NCK-interacting kinase inhibitor. Scientific Reports. 2016; 6:33534.
Walk-Vorderwulbecke V, Pearce K, Brooks T, Hubank M, Zwaan cM, Edwards AD, Ancliff P. Targeting acute myeloid leukemia by drug-induced c-MYB degradation. Leukemia. 2018; 32:882- 9.
The following Case Report is from a 63 yr old man who was initially diagnosed with BRAF-positive maliginant melanoma in 2020. Chemotherapy put him into remission but the cancer came back in 2023, which is when he tried a different approach using fenbendazole.
In July of 2020 I had noticed a growth on my hip. It was biopsied and was determined to be a BRAF mutation-positive melanoma which had spread to some of my lymph nodes. My oncologist recommended chemotherapy, tafinlar, which I took for a year and it worked as I was put into remission.
Fast forward to late August 2023: I had a PET scan that showed that the cancer had returned with metastases to my lower abdomen, back next to my spine, leg and four tumors in my ureter. I had follow up biopsies that confirmed that the DNA in the tumors were the BRAF-positive melanoma cells that had returned and had spread.
In December 2023 the tumors had disrupted my ureter causing problems with urination, so I had surgery to remove that tumor. My oncologist wanted me to hold off on scheduled immunotherapy treatments with opdivo (Nivolumab) until I had recovered from the effects of the surgery. My oncologist also stated that nivolumab was by no means a cure of any kind but that it might give me some more time.
A few days later my wife heard about fenbendazole and this Substack through a friend of a friend. I was able to track that person down and he was kind enough to speak with me. He was very encouraging and, because my doctor said that immunotherapy was no cure and I had a traditional treatment-free window ahead of me while recovering, so while I was skeptical of fenbendazole there was really no reason not to give fenbendazole a shot.
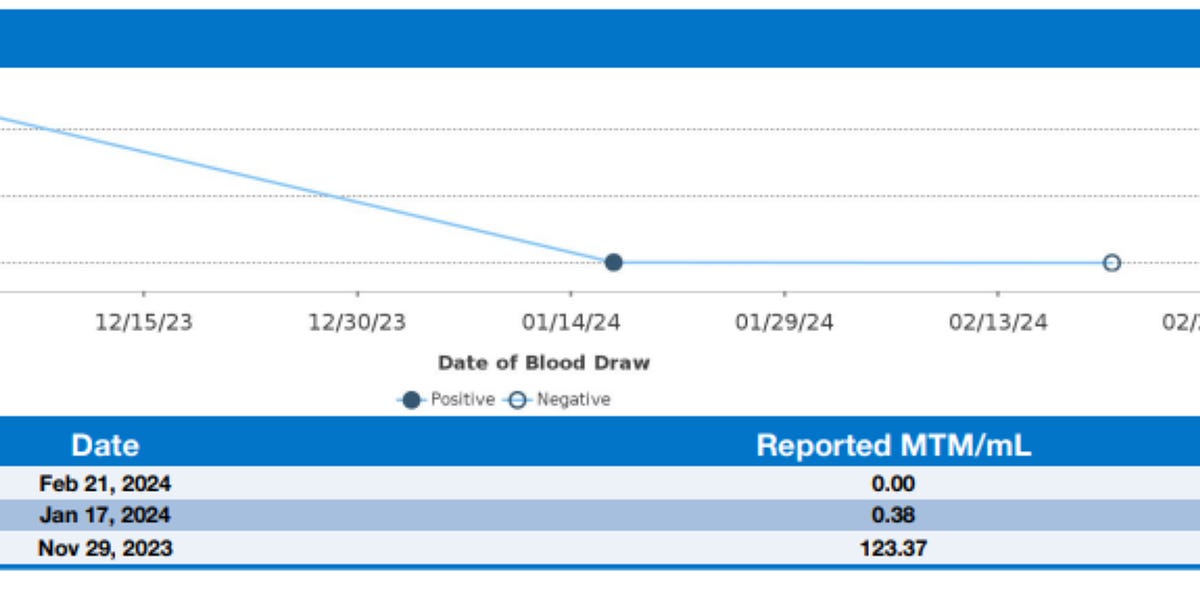
I started taking fenbendazole 222 mg once or twice per day around mid-December 2023. As you can see from the graph of the blood tumor markers (which measures the amount of the tumor’s DNA in the blood) for my cancer, that before I started any fenbendazole treatments, that on Nov 29 it was 123.37. Less than 7 weeks later, on Jan 17, 2024, it had dropped to 0.38 and about a month later on Feb 21, 2024 it was 0, zero!
In that time period I did have two immunotherapy treatments but those are not the likely cause of my cancer disappearing for two reasons. First, my oncologist said immunotherapy wouldn’t cure me, just give me more time, maybe. And, two, last week when my oncologist came in to the room to tell me about the Feb 21 blood test she said “I don’t know how to tell you this but there is no evidence of cancer. Nothing. This just doesn’t happen after only two treatments.” Of course she knows nothing about fenben because I didn’t tell her I was taking it.
J. F., Ozark, Missouri, March 7, 2024
Q: How old are you? Weight? How do you feel?
A: 63 years old, 232 lb. when this started. About 170 lbs now and gaining my weight back, which is good. I feel wonderful!
Q: What brand of fenbendazole were you taking? And how many times per day? Any side effects?
A: It is TheLife brand of fenbendazole, and my wife bought it on Amazon. I took 222 mg once or twice a day. There were no side effects from the fenben. FYI I saw the health insurance bill for the immunotherapy drug, opdivo, it was $72,000. My wife spent $60 on the fenbendazole, which is what worked!
Q: Are you still taking fenben?
A: Yes. I take 222 mg once per day.
Summary
Congratulations to J. F. for taking matters into his own hands and having a tremendous outcome. We wish him the best going forward and are greatly appreciative of his sharing his experiences so that others faced with similar circumstances may benefit.
BRAF mutations are not restricted to melanomas alone. Again, according to Johns Hopkins, the cancers associated with the BRAF gene mutation are not specific to one part of the body or a certain cell type and include hairy cell leukemias, non-Hodgkin lymphomas, thyroid cancer, ovarian cancer, lung adenocarcinoma, colorectal cancer and certain brain cancers, including glioblastoma, pilocytic astrocytoma, and pediatric low-grade glioma.
In this Case Report, a very aggressive BRAF-positive variant of melanoma appears to have been eradicated by fenbendazole. This report is yet another example of fenbendazole eradicating purported “aggressive” forms of untreatable cancers including triple-negative breast cancers as we’ve previously reported. These results in humans should not be surprising given the wealth of pre-clinical animal data on fenbendazole and mebendazole indicating that these outcomes are to be expected (Doudican, et al., 2013; Simbulan-Rosenthal, et al., 2017 for example, regarding melanomas).
Because J. F. did receive another treatment there could be alternative explanations for his tremendous outcome. First, J. F. did receive two doses of immunotherapy (nivolumab). It is a possibility that that protocol was effective for him in eradicating his BRAF-positive melanoma. Unique individual differences aside, such an outcome would be highly unlikely given the published data on nivolumab as well as J. F.’s oncologist’s expectations and advice.
Second, it is possible that there was an interaction between the two doses of nivolumab, and fenbendazole resulting in a synergistic effect that eradicated the cancer. If this is what happened, it is a major discovery to be further investigated.
Third, fenbendazole alone was the effective anti-cancer agent that eradicated the BRAF-positive melanoma cells. Skimming through the twenty or so references below examining fenbendazole/mebendazole’s role in cancer treatment, indicates that fenbendazole is both necessary and sufficient to achieve the results in experimental pre-clinical models of cancer that J. F. obtained in his own self-treatment cancer clinical trial.
Because the BRAF gene mutation is most likely caused by an environmental factor that led to the mutation, presuming that the factor responsible for the mutation can be eliminated, the possibility of a true cure for BRAF-positive cancers using fenbendazole may be at hand. More on this idea later as we present a more complete discussion as to what cancer is and isn’t in the context of an agent like fenbendazole.
References
Bai RY, Staedtke V, Rudin CM, Bunz F, Figgins GJ. Effective treatment of diverse medulloblastoma models with mebendazole and its impact on tumor angiogenesis. NeuroOncology. 2015; 17:545-54.
Chiang RS, Syed AB, Wright JL, Montgomery B, Srinivas S. Fenbendazole enhancing anti-tumor effect: A case series. Clin. Oncol. Case Rep. 2021; 4:2.
Dobrosotskaya IY, Hammer GD, Schteingart DE, Maturen KE, Worden FP. Mebendazole monotherapy and long-term disease control in metastatic adrenocortical carcinoma. Endocr. Pract. 2011; 17(3):e59-e62.
Doudican NA, Byron AA, Pollock PM, Orlow SJ. XIAP downregulation accompanies mebendazole growth inhibition in melanoma xenografts. Anti-Cancer Drugs. 2013; 24:181-8.
Gallia GL, Holdhoff M, Brem H, Joshi AD, Hann CL, Bai RY, et al. Mebendazole and temozolomide in patients with newly diagnosed high-grade gliomas: results of a phase 1 clinical trial. Neuro- Oncology Advances. 2021; 3:1-8.
Guerini AE, Triggiani L, Maddalo M, Bonu ML, Frassine F, Baiguini A, Alghisi A. Mebendazole as a candidate for drug repurposing in oncology: An extensive review of current literature. Cancers. 2019; 11:1284.
Meco D, Attina G, Mastrangelo S, Navarra P, Ruggiero A. Emerging perspectives on the antiparasitic Mebendazole as a repurposed drug for the treatment of brain cancers. Int. J. Mol. Sci. 2023; 24:1334.
Nygren P, Larsson R. Drug repositioning from bench to bedside: tumor remission by the antihelmintic drug mebendazole in refractory metastatic colon cancer. Acta Oncol. 2014; 53(3):427-8.
Nygren P, Fryknas M, Agerup B, Larsson R. Repositioning of the anthelmintic drug mebendazole for the treatment for colon cancer. J. Cancer res. Clin. Oncol. 2013; 139:2133-40.
Pantziarka P, Bouche G, Meheus L, Sukhatme V, Sukhatme VP. Repurposing drugs in oncology (ReDO) - mebendazole as an anti-cancer agent. Ecancer. 2014; 8:443.
Patel, H., Yacoub, N., Mishra, R., White, A., Long, Y., Alanazi, S., & Garrett, J. T. (2020). Current Advances in the Treatment of BRAF-Mutant Melanoma. Cancers, 12(2), 482.
Pinto LC, Soares BM, de Jusus Viana Pinheiro J, Riggins GJ, Assumpcao PP, Burbano RM, Montenegro RC. The anthelmintic drug mebendazole inhibits growth, migration and invasion in gastric cancer cell model. Toxicology in Vitro. 2015; 29:2038-44.
Pinto LC, de Fatima Aquino Moreira-Nunes C, Soares BM, Rodriguez Burbano RM, de Lemos JA, Montenegro R. Mebendazole, an antiparasitic drug, inhibits drug transporters expression in preclinical model of gastric peritoneal carcinomatosis. Toxicology in Vitro. 2017; 43:87-91.
Sasaki JI, Ramesh R, Chada S, Gomyo Y, Roth JA, Mukhopadhyay T. The anthelmintic drug mebendazole induces mitotic arrest and apoptosis by depolymerizing tubulin in non-small cell lung cancer cells. Molecular Cancer Therapeutics. 2002; 2:1201-9.
Simbulan-Rosenthal CM, DDakshanamurthy S, Gaur A, Chen YS, Fang HB, Abdussamad M, et al. The repurposed anthelmintic mebendazole in combination with trametinib suppresses refractory NRASQ61k melanoma. Oncotarget. 2017; 8:12576-95.
Tan Z, Chen L, Zhang S. Comprehensive modeling and discovery of mebendazole as a novel TRAF2- and NCK-interacting kinase inhibitor. Scientific Reports. 2016; 6:33534.
Walk-Vorderwulbecke V, Pearce K, Brooks T, Hubank M, Zwaan cM, Edwards AD, Ancliff P. Targeting acute myeloid leukemia by drug-induced c-MYB degradation. Leukemia. 2018; 32:882- 9.