I think some of the doagnoses are mis diagnosed as the doctors are paid to not diagnose glycophosphate as an allergy. Big pharma makes big money on needless drugs in some cases. But i find it odd some people diagnosed with disorders have them disappear when they eat food traveling abroad. So it is glycophosphate or gmo foods at fault
Symptoms are similar, but true celiac diagnosis is based on blood tests and biopsy. Celiac is an autoimmune disease that causes destruction of intestinal villi. In some people the symptoms are mild enough at times that food with less gluten, for example overseas, might cause fewer symptoms, but the silent damage continues with even minute exposure.
Glyphosate/gmo have their own serious issues, but it is *not* the same.
This article has a good explanation (it is longer than I was able to post)
Celiac disease, gluten sensitivity, wheat allergy and gluten intolerance: What’s the difference? Pediatric gastroenterologist Dr. Ritu Verma explains.

www.uchicagomedicine.org
Two conditions that seem like celiac disease, but aren't
January 17, 2020
Written By Dr. Ritu Verma
An estimated 1 in 100 people worldwide have celiac disease, a disorder where consuming any type of gluten can damage the small intestine. Gluten is a protein found in wheat, rye and barley, which are common ingredients in breads, pastas and cereals.
Despite awareness efforts, celiac disease is often confused with other gluten-related disorders — like non-celiac gluten sensitivity (NCGS) or a wheat allergy. Both seem similar to celiac disease, but are different conditions.
While the symptoms may be similar, these distinct medical conditions require different types of care. We asked pediatric gastroenterologist Ritu Verma, MD, medical director of the thyroid disorders, low bone density and intestinal cancers. Diagnosis requires a positive celiac blood test and small intestine biopsy.
Symptoms: They’re extremely varied. They can be gastrointestinal (diarrhea, abdominal pain, etc.), non-gastrointestinal (chronic headaches, certain rashes, poor growth, etc.), or a person could be asymptomatic.
What sets it apart: It involves complete gluten restriction and careful avoidance of cross-contamination. It also can run in families, so it’s important that family members be screened. It can develop at any age, so both adult and pediatric doctors can treat it.
Treatment: Lifelong gluten restriction and follow-up care. A dietitian and medical providers need to assist with information about food choices, reading labels and lifestyle adjustments.
Non-celiac gluten sensitivity (NCGS)
What it is: Gastrointestinal (GI) and non-GI problems related to gluten consumption, but blood tests and biopsies test negative for celiac disease and wheat allergies.
Symptoms: Similar to celiac disease, with GI and non-GI symptoms like abdominal pain, bloating and fatigue.
What sets it apart: Blood tests are negative and biopsies are normal, despite eating gluten. Some gluten consumption is OK, up to the level that causes symptoms. People with NCGS don’t have to be as restrictive with gluten and cross contamination as people with celiac disease do.
Treatment: Despite testing negative for celiac, patients still experience symptoms. We help identify the threshold amount of gluten causing the symptoms, and remove it from the diet. Symptoms will improve on a gluten-free diet, but it’s still important to meet with a dietitian to avoid vitamin and nutritional deficiencies.
Gluten (wheat, rye or barley) allergy
What it is: An immediate allergic reaction to foods containing wheat, rye or barley.
Symptoms: Itching, hives, trouble breathing or anaphylaxis (a life-threatening reaction), nausea, abdominal pain, itching and swelling lips or tongue.
What sets it apart: It’s the only gluten-related reaction helped by EpiPens (injectable epinephrine). Patients are treated by allergists rather than gastrointestinal doctors.
Treatment: Avoidance of allergy-causing food. An EpiPen could be used to stop the allergic reaction. Dietitians can help patients remove the problematic gluten from their diet.
Dr. Ritu Verma and dietitian Macy Mears answer questions about celiac disease
Video Transcript
Celiac disease is an autoimmune disease that means people who have it and eat gluten will damage their small intestine. And when people eat things like wheat, rye, or barley, their body reacts, and that reaction is harmful to their small intestine. Millions of people are impacted by celiac disease. Do you or a loved one have celiac, and how can you deal with it? It's coming up right now on At the Forefront Live.
Today on At the Forefront Live, physician Ritu Verma and dietitian Macy Mears joins us to discuss celiac. And remember, you can ask questions of our experts, so make sure you start typing in the comments section at the bottom of the screen. And our final reminder is the program is not designed to take the place of a visit with your physician. So for serious things, go see your doctor, but ask lots of questions today because we've got some great experts on. Thank you for being on the program.
Thank you.
Appreciate you being here, and we'll just start off with kind of the basics and if you can describe to us what celiac disease.
So celiac disease is an autoimmune disease, contrary to what people think that it's an allergy, but it truly is an autoimmune disease, just like someone has multiple sclerosis or type one diabetes, and there's also a genetic component to that. So based on the genes, it's an autoimmune disease, and it occurs in people who then will eat gluten, which then causes damage to your small intestine.
And when you say damage to the small intestine, what does it do?
So the small intestine, even though it's called small intestine, is really a long organ, but it has these surfaces on the inside which have these things called villi. They're finger-like projections that help absorb nutrition. And what happens with celiac disease is the gluten then causes damage to the lining of these cells, to the villi, and the villi sort of shrivel up. Depending on how severe the disease is, this is mild shriveling to total flattening of the small intestine, and that hinders the absorption of nutrition.
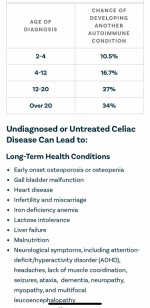
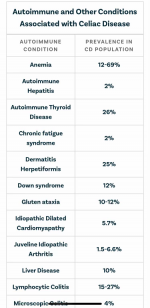
And then the second part that happens with the disease is there is the intestinal part, and then the second is it can cause other autoimmune diseases. And that's why it's more a genetic autoimmune disease.
So it can be a pretty serious situation for people who suffer from it.
Absolutely. If it's not treated, not recognized in time, yes, it can cause a lot of complications.
Now it's interesting. When we talk about celiac disease, I think there's a lot of common misconceptions. And Macy, I'm glad you're here today because as a dietitian, you're a very important part of the team working with folks who have celiac. When do you come into the equation?
So it's usually when there's a known diagnosis. And at least for our clinic it works when the diagnosis is known. Then you make an appointment with the physician and automatically also see me because it is so food based, and our treatment right now is a gluten-free diet. So yes, I am very involved.
And it's really important for people to remember that part of the team here, a very important part of the team is the dietitian since it is a diet-related disease.
Well, and that's interesting, and I think it certainly bears repeating because one of the things we do here at UChicago Medicine, we believe in the team-based approach, and you two are a perfect example of that. And that's really critical to the correct care of our patients.
Absolutely. I think that one of the most important things that we can do is to have patients come in, see the physicians, see the dietitian. In some conditions we also need a psychologist. And the other beauty of being here at the University of Chicago is that as you get older, you have a transition that you can actually go and see an adult gastroenterologist as well and an adult dietitian. It goes across the continuum from pediatrics to adult being here at the University of Chicago.
So as we talk about pediatrics, when do we commonly see children first diagnosed with celiac? Is it something that starts right away, or is it something that happens a little later in life?
So usually a child has to start eating gluten, and so it usually occurs somewhere between 1 and 1/2, 2, depending on the eating habits in a particular family. You would say we probably see most of the children between two, three and older.
And then it really can be at any age. You can have a teenager be diagnosed with celiac disease for the first time. You can have an adult diagnosed with the disease for the first time as well.
And when you're dealing with these kids, Macy, I imagine it's probably challenging, particularly the younger children, to even have them understand that they have to change lifestyle. Of course mom and dad are a critical part of that, but how do you do that?
Yeah, that is a really good point just working with peds because each patient is different anyway. But also-- I know this is something we do-- you have to kind of channel yourselves to be like, OK, what will make this child change or realize that it's important to be the different kid at school or have to have a different snack? So I think just talking through it and really getting the whole family involved-- so patient centered but very family focused helps because then it does go along that continuum as they keep growing and understanding more.
It seems like we see a lot in the news and read a lot online about celiac disease, and we're hearing more and more about gluten-free diets. How common is this today?
So celiac disease, it's about 1% of the population. In some populations you see 1 in 80. In some areas, it's a prevalence of 1 to 100. However, I think there's a lot of people who don't have celiac disease but are on the gluten-free diet. And the other things to think about is if you have an allergy to gluten, any part of the gluten. And gluten, of course, is wheat, rye, and barley, so you could have an allergy to one of these products. And then there is, of course, nonceliac gluten sensitivity.